Bipolar Disorder Seed Grants for Faculty
Supported by the Dauten Family Foundation and Sandra Lee Chen and Sidney Chen, the HBI Bipolar Disorder Seed Grant Program funds research relevant to the basic understanding and treatment of bipolar disorder at Harvard University and its affiliated hospitals. It funds innovative, visionary projects with new ideas and approaches that address fundamental questions about the disorder and may not attract funding from conventional sources.
The program was launched in 2015 with the vision of the Dauten family. It has issued over 90 grants and led to five symposia to date. This year, with the Dauten and Chen families’ generous gifts coming together, the program has grown to provide two-year seed grants of $174,000 each, supporting the launch of 11 diverse projects spanning the realms of basic, translational and clinical research.
We are delighted to announce below the 2025 awardees! Scroll down to learn more about their projects.
2025-2026 Awards
 Paola Arlotta, PhD
Paola Arlotta, PhD
Professor, Department of Stem Cell & Regenerative Biology,
Harvard University
Human “Brain Organoids” As Avatars To Understand Individual Variation in Treatment Response in Bipolar Disorder
Despite the urgent need for effective treatments, the success rate for new drugs for Bipolar Disorder (BD) and other neuropsychiatric conditions remains low. One difficulty is that individual humans vary in their responses to both disease and treatment: in BD, the most effective first-line treatment, lithium, is fully efficacious in only about 30% of patients, and even among “lithium responders”, ~75% experience profound side effects.
Our lab has created a cell culture model of human brain tissue, human brain “organoids”. In pilot work, we have created brain organoids using stem cell lines derived from BD patients who either respond well to lithium in the clinic (“lithium responders”), or who do not respond (“lithium non-responders”). Based on these promising pilot results, here we propose to 1) test whether these organoids can replicate individual differences in patient response to BD therapeutics they received during treatment, and to 2) set up a proof-of-concept screen of known and candidate BD therapeutics, aiming to identify compounds that ameliorate disease signatures in organoids. This work seeks to establish brain organoids as a powerful experimental system that can replicate clinical differences in drug response between individual patients, to empower both disease research and drug development in BD.
 Catherine Dulac, PhD
Catherine Dulac, PhD
Professor, Department of Molecular and Cellular Biology,
Harvard University
Neuroimmune Interactions Underlying Bipolar Disorder
Recent advances suggest a critical link between dysregulated immune activity and the pathophysiology of numerous neuropsychiatric conditions, including bipolar disorder. However, the mechanisms by which this immune dysregulation impacts brain circuits and behavior remain poorly understood. The hypothalamus is a key component of the dysfunctional HPA axis in bipolar disorder and mediates the regulation of many social behaviors and physiological functions affected by bipolar disorder. Accordingly, we will investigate how distinct classes of immune signals influence behavior and neural activity in wild type and established mouse models of bipolar disorder. Further, we will comprehensively examine with cell-type resolution the origin and effect of different types of immune signaling in the hypothalamus of WT and bipolar models. This study will provide crucial insights into the interplay between immune dysregulation, neural activity, gene expression and behavior in bipolar disorder.
 Susan Dymecki, MD, PhD
Susan Dymecki, MD, PhD
Professor, Department of Genetics,
Harvard Medical School
A Brain Circuit and Cell Behavior Contributing to the Seasonality Patterns of Affective Disorders
Bipolar disorder is a chronic illness with alternating manic and depressive episodes that disrupt mood, circadian rhythms, and energy levels. An emerging framework posits that bipolar disorder is primarily a disorder of sleep and circadian rhythms. These disturbances often predict mood episodes, with a seasonal pattern to disease progression influenced by daylength (photoperiod). Depressive episodes are more common in fall/winter, and mania in spring/summer, with mood cycling frequently triggered at transitions between long and short days (and vice versa), or by trans-meridian travel and shift work. Underlying mechanisms are largely unknown. Our research aims to identify molecules, cells, and brain circuits involved in adaptation to changes in photoperiod, seeking to identify novel interventions. We found a specific brain circuit in mice, involving serotonin-glutamate neurons (mrEn1-Pet1 neurons), that regulates sleep/wake and circadian synchronization to daylength change. We hypothesize that mrEn1-Pet1 neurons act like switchboards with opposing, state-dependent roles in circadian adaptation. These roles, involving glutamate for timely adaptation to photoperiods and serotonin for protecting against light perturbation effects, may be independent pharmacologically and separately tunable. We will analyze serotonin versus glutamate signaling in organismal adaptation to photoperiod change and elucidate circuits that may be tapped therapeutically to ameliorate affective disorder symptoms.
 Michael E. Greenberg, PhD
Michael E. Greenberg, PhD
Professor, Department of Neurobiology,
Harvard Medical School
Aberrant Astrocyte Glucocorticoid Receptor Signaling in Bipolar Disorder
Stress is an important contributor to bipolar disorder (BD) and related psychiatric illness. We recently uncovered an unexpected role for stress hormone signaling within astrocytes—a glial cell type that serves to modulate neuronal physiology and plasticity—in mediating visual circuit maturation in juvenile animals. This project will test the role of this signaling mechanism in the maturation of key BD-implicated brain regions and whether dysregulation of this regulation may contribute to BD. Together, these studies will advance understanding of the role of early stress in BD etiology and provide opportunities for the development of therapeutic strategies for treating BD.
 Jun Huh, PhD
Jun Huh, PhD
Associate Professor, Department of Immunology,
Harvard Medical School
How the Immune System and Gut Bacteria May Influence Bipolar Disorder
This study explores how the immune system and gut bacteria might contribute to symptoms of bipolar disorder, a mental health condition that causes extreme mood swings. We plan to use a special type of mouse model, ANK3 knockout, that shares some key features of the disorder. The research has two main goals. First, we will examine how gut microbes and immune responses differ in these mice compared to typical mice. Second, they will test whether changes in gut bacteria or immune activity affect the mice’s mood-related behaviors. The team will use well-established behavioral tests to look for signs of anxiety or depression in the mice. They will also study brain and body signals linked to inflammation and mood regulation. Both male and female mice will be included to see if there are any differences based on sex. The hope is to discover new biological links between the gut, the immune system, and the brain. These findings could lead to better treatments for people living with bipolar disorder, especially those who don’t respond well to current medications.
 William A. Carlezon Jr., PhD
William A. Carlezon Jr., PhD
Professor, Department of Psychiatry,
McLean Hospital and Harvard Medical School
Induction of Mania-Like Signs in Mice by Perinatal Immune Activation via TLR7, a Gene Implicated in Bipolar Disorder
Accumulating evidence shows that immune system activation during early development can produce effects on the brain and behavior that persist over the lifespan. These findings have stimulated interest in Toll-Like Receptors (TLRs), a class of cell-surface receptors that regulate immune responses. While there are many TLR subtypes, the Carlezon lab has focused on TLR7, which is encoded by a gene (TLR7) linked to bipolar disorder (BPD). In mice, transient activation of TLR7 around the time of birth triggers the later emergence of a unique behavioral profile, characterized by reduced anxiety, elevated locomotor activity, and fragmented social interactions (i.e., increases in the number of interactions together with decreases in their duration). This profile resembles aspects of mania, a key feature of BPD that is characterized by mental and physical hyperactivity, elevated mood, irritability, increases in reward-seeking activities, and a reduced need for sleep. In this project, the Carlezon lab will determine if perinatal TLR7 activation in mice also increases sensitivity to reward and decreases time spent asleep, using procedures and measurements that align closely with those used in humans. These studies will enhance our understanding of how TLR7 function affects the development of brain circuits that regulate the symptoms of BPD, and provide new insight on whether the key features of mania are linked mechanistically. They may also yield an improved animal model that can be used to screen new treatments for BPD.
 Jordan Farrell, PhD
Jordan Farrell, PhD
Assistant Professor, Department of Neurology,
Boston Children’s Hospital and Harvard Medical School
Hypothalamic Control of Manic-Like States
In a novel setting, mammals typically ramp up exploratory behavior and increase the excitability of the cortex, facilitating plasticity so that we can adapt to new environments. In bipolar disorder (BD), this process may not appropriately adapt to familiarity, underscoring the need to understand the mechanisms regulating exploration and changes in cortical excitability. Although typically studied separately, exploration and cortical excitability is tightly linked. Our recent findings suggest that a small region of the hypothalamus, called the supramammillary nucleus, is a critical circuit node linking these processes and is ripe for interrogation in BD. Under normal conditions, this brain area is recruited by novelty and potently controls exploratory behavior and the firing of neurons across cortical circuits. To understand what might go wrong in this circuit in BD, we utilize mice that have a mutation in a gene that is strongly associated the occurrence of a clinical BD diagnosis, and compare these mice to their unaffected littermates. By studying and manipulating this brain area in a model of BD, this work could uncover a critical chokepoint to control BD-related behaviors and a potential target for neuromodulation.
 Christopher Harvey, PhD
Christopher Harvey, PhD
Professor, Department of Neurobiology,
Harvard Medical School
Multiplexing Measurement of Neural Activity and Neuromodulation in Bipolar Disorder
Therapies for bipolar disorder include drugs that modify the function of neuromodulators in the brain, including serotonin and dopamine. Emerging evidence suggests that multiple neuromodulatory systems interact in complex ways for the natural progression of the disorder and its treatment. However, due to technical limitations, we currently know little about the interactions between dopamine and serotonin in bipolar disorder and how their interactions affect the function of the brain during the disorder. We propose to develop a method to measure simultaneous changes in serotonin, dopamine, and brain activity in mice. Then, in genetic mouse models of bipolar disorder, we will investigate how these neuromodulators, and importantly their interactions, are altered in the cerebral cortex. Our work has the potential to reveal new dimensions of the disruptions in neuromodulation and its effect on brain function in bipolar disorder. Furthermore, the methods we will develop have the potential to generalize to other neuromodulatory systems and to reveal how disruptions in neuromodulation interact with the complex genetics underlying bipolar disorder.
 Daniel Hochbaum, PhD
Daniel Hochbaum, PhD
Assistant Professor, Department of Medicine,
Beth Israel Deaconess Medical Center and Harvard Medical School
Thyroid Hormone Modulation of Dopamine Signaling as a Molecular and Circuit Mechanism Underlying Mania and Depression
Both thyroid hormone and the neuromodulator dopamine have been implicated in the underlying genetics, physiology, behavioral phenotypes, and treatment of bipolar disorder. In this grant, we propose that these nominally separate systems can interact in the brain to produce characteristic symptoms of bipolar disorder.
We recently discovered that thyroid hormone, a critical metabolic regulator in organs throughout the body, enters the brain and induces plasticity of neural circuits to promote exploratory behaviors. Conversely, loss of brain thyroid signaling can diminish exploratory behaviors. The bidirectional action of thyroid hormone in the brain parallels the symptoms of depression and mania common in bipolar disorder, where exploratory, risky, behaviors are either neglected or over-expressed. Dopamine neurons are key to mediating exploratory and risky behaviors, and we find that these neurons contain all the molecular machinery necessary to respond directly to thyroid hormone. The goal of this grant is to dissect the interaction of thyroid and dopamine signaling to uncover molecular mechanisms driving exploratory behaviors, with the ultimate goal of identifying avenues for therapeutic treatment of bipolar disorder.
 Bernardo Sabatini, MD, PhD
Bernardo Sabatini, MD, PhD
Professor, Department of Neurobiology,
Harvard Medical School
Investigating the Function of all Identified Bipolar Disorder Risk Genes in the Mouse Brain
Human genetic studies have identified a growing number of risk genes in bipolar disorder (BD). However, translating these genetic associations into an understanding of how the disease arises and potential therapeutic targets has been challenging. One major obstacle has been the slow process of studying genes in animal models; BD arises developmentally and likely involves the interplay of many cell types, thus requiring modeling in an intact brain. Yet the generation and analysis of animal models is labor-intensive and slow. As a result, of the more than 60 genetic loci implicated in BD, only a handful have been investigated in vivo. We propose to address this bottleneck by studying the function of all identified bipolar risk genes. We will take advantage of a platform we recently developed to generate mosaic mice with different genes disrupted in different cells. We will apply this approach to study the cellular impact of disrupting each BD risk gene and search for shared disease pathways. This project will provide a systematic look at the function of BD risk genes in the context of an intact animal brain.
 Louisa Sylvia, PhD
Louisa Sylvia, PhD
Associate Professor, Department of Psychiatry,
Massachusetts General Hospital and Harvard Medical School
Impact of Time-Restricted Eating on Weight Loss, Mood and Circadian Rhythms in Patients with Bipolar Disorder
Individuals with bipolar disorder (BD) face a higher risk for obesity, which is associated with poorer health outcomes. Time-restricted eating (TRE) is a novel dietary intervention that limits food intake to a 6 to 10-hr daytime ‘eating window’ (e.g., eating only between 8am to 6pm). TRE has been shown to improve weight loss with promising data that it may also improve mood, cognition, and sleep. It is expected that TRE may help regulate one’s daily rhythms, a common factor that has been shown to be disrupted in both obesity and BD. Despite its potential, no studies have examined TRE in individuals with bipolar depression and comorbid obesity. To address this gap, we seek to examine the effect of an 8-week TRE intervention on weight loss and secondary health outcomes in individuals with BD and whether these associations are due to improvement in circadian rhythms. We will enroll 48 adults with BD, currently experiencing at least mild depressive symptoms and obesity. These participants will be randomly assigned to either TRE or a wait list control to examine the impact of TRE on body weight, secondary health outcomes (e.g., mood, quality of life, cognition) as well as circadian rhythms.
2024-2025 Awards
Ovidiu C. Andronesi, MD, PhD
Associate Professor of Radiology,
Harvard Medical School and Mass. General Hospital
Aapo Nummenmaa, PhD
Assistant Professor of Radiology,
Harvard Medical School and Mass. General Hospital
Michael E. Henry, MD
Associate Professor of Psychiatry,
Harvard Medical School and Mass. General Hospital
Image-Guided Quantitative TMS as a Therapy for Bipolar Disorder
Many individuals with bipolar disorders have functional impairments which negatively impact long-term prognosis. Pharmacological treatments are primarily targeted towards improvement of mood symptoms, but few treatments improve cognitive dysfunction. There is urgent clinical need to improve existing treatments and develop novel therapeutic options that are safe and improve other features of bipolar disorders, including cognitive dysfunction. There is a growing interest in brain stimulation as an add-on or alternative to existing treatments for bipolar disorders. Transcranial magnetic stimulation (TMS) is particularly appealing since it can be done without anesthesia, does not have the side effects of other stimulations, does not require surgery to implant electrodes, and stimulation can be focused and quantified through neuroimaging. The efficacy of TMS has been shown for major depressive episodes in patients who didn’t respond to other medication, however it is unclear to what extent this applies to bipolar patients. In this project we will establish imaging biomarkers to optimize TMS in bipolar patients for precision-personalized treatment. We will use robotically navigated quantitative TMS to precisely target and dose stimulation. Using novel functional and neurotransmitter imaging we will identify brain regions that can be targeted by TMS and measure objective-response rate to predict clinical response.
 Michael Crickmore, PhD
Michael Crickmore, PhD
Assistant Professor of Neurology,
Harvard Medical School
A Genetic Model For Understanding Dopamine Receptor Activity Cycles
An individual’s D2 dopamine receptor (D2R) levels are predictive for bipolar disorder. Drugs that are D2R antagonists are a frontline treatment for the manic phase of bipolar disorder, which is associated with increased D2R availability. The D2R is notoriously subject to use-dependent desensitization, pointing to cycles of D2 receptor inactivation and recovery as a possible underlying driver of the depressive-manic cycling in bipolar disorder. To understand the mechanisms behind D2R sensitivity cycles we have developed behavioral and imaging assays to investigate the changing activity of the D2R in response to endogenous dopamine release as animals transition through different natural behavioral states. Previous mechanistic work on D2R desensitization has almost exclusively been in the context of non-physiological agonist- or drug-induced, widespread increases in dopamine. In this project we plan to use fruit fly neurogenetics to develop a detailed understanding of the pathways that set D2R desensitization and recovery cycles in the context of natural behavior. This system will help to develop new hypotheses for stabilizing dopamine signaling in bipolar disorder.

 Darin Dougherty, MD, MSc
Darin Dougherty, MD, MSc
Associate Professor of Psychiatry,
Harvard Medical School and Mass. General Hospital
Tina Chou, PhD
Assistant Professor of Psychology,
Harvard Medical School and Mass. General Hospital
Low-Intensity Focused Ultrasound of the Amygdala as a Therapy for Bipolar Disorder
Brain stimulation has shown great promise in psychiatry. Transcranial magnetic stimulation (TMS) has been FDA approved for depression and obsessive-compulsive disorder. Deep brain stimulation (DBS) has also been FDA approved for treatment-resistant OCD. These stimulation methods have advantages and disadvantages; TMS does not require neurosurgery but is limited to stimulating regions at the surface of the brain. DBS can stimulate deeper brain regions but requires invasive neurosurgery and long-term maintenance of the device. A newer form of brain stimulation is transcranial focused ultrasound (tFUS). tFUS allows access to deep brain regions without the use of neurosurgery. Due to the role of a deep brain region, the amygdala, in bipolar disorder, we propose an initial feasibility study targeting the amygdala with tFUS to change brain network activation during emotion regulation and resting-state network activity in individuals with bipolar disorder. The results from this study could lead to the development of a novel intervention for individuals suffering from bipolar disorder.

 Fei Du, PhD
Fei Du, PhD
Associate Professor of Psychiatry,
Harvard Medical School and McLean Hospital
Mark Halko, PhD
Assistant Professor of Psychiatry,
Harvard Medical School and McLean Hospital
Unraveling Brain Circuit Disruptions in Bipolar Disorder with TMS and Neuroimaging Approaches
Bipolar disorder (BD) is characterized by a history of hypo/manic episodes, periods of elevated or irritable mood and energized behaviors which may alternate with episodes of depression. The treatments often face issues of unresponsiveness and significant side effects, highlighting the need for innovative therapeutic approaches. BP is increasingly recognized as a disorder of brain networks or neuronal communications, reliably characterized by disrupted cerebellar-cortical circuitry and abnormalities in the glutamate and gamma-aminobutyric acid systems, along with abnormal mitochondrial function. This study utilizes a causal approach to investigate these systems, using transcranial magnetic stimulation to manipulate cerebellar-cortical circuitry to assess metabolic and functional changes, as a precursor to the development of novel circuit-specific treatment paradigms in BP patients and/or biomarkers for effective personalized neurointervention.
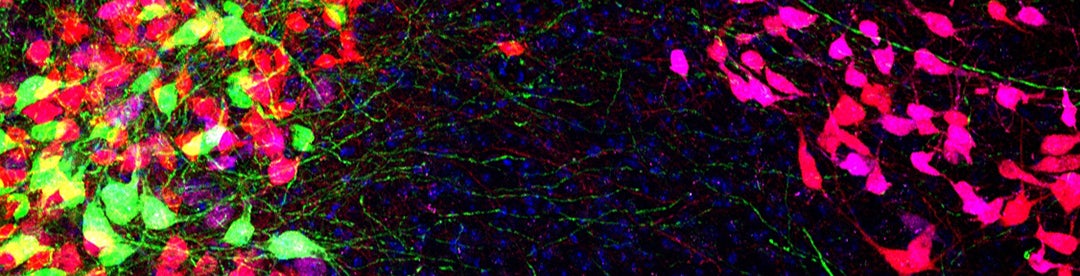
 Gordon Fishell, PhD
Gordon Fishell, PhD
Professor of Neurobiology,
Harvard Medical School
Identifying and Repairing Brain Function in a Model of Bipolar Disorder
At a molecular level, the loss of the Akap11 gene can cause bipolar disorders. Our lab is interested in examining interneurons in mice lacking Akap11 gene function. Interneurons are a particularly promising target for underlying bipolar disorders, as they function by allowing us to focus on critical information, while reducing unnecessary noise. We hypothesize that loss of this gene in interneurons plays a crucial role in this disease. Importantly, throughout the cortex, the same interneuron classes are found across all cortical layers. Thus, we can focus on any particular brain region and extrapolate these findings to all other areas. We have chosen to look at visual cortex, the brain area where signaling is best understood and comparing signaling in control animals versus those lacking Akap11. By understanding how loss of this gene affects interneuron function in the visual system, we believe we can determine how interneuron defects may contribute to bipolar disorder in areas of the brain directly impacted in this disease. Our hope is that this will lead to treatments where we can improve the symptoms experienced by individuals with bipolar disorder.
 Robert Gonzalez, MD
Robert Gonzalez, MD
Member of the Faculty,
Harvard Medical School and Brigham and Women’s Hospital
Examining the Relationships Between Locomotor Activity and Mood State in Bipolar Disorder
Bipolar disorder (BD) is a chronic and disabling illness. There remains an unmet need in establishing disease monitoring markers for the disorder. Actigraphy is an easily accessible, non-invasive tool for measuring locomotor activity. Disturbances in locomotor activity are a core feature of BD and have been associated with mood states, clinical characteristics, and treatment response. Our previous actigraphy-based protocol including 105 BD patients demonstrated that less robust circadian rhythmicity of locomotor activity was associated with a greater severity of mania and specific symptoms related to this syndrome. Utilizing data from this existing, well-characterized sample, we will implement novel and sophisticated modeling methods to identify and quantify complex locomotor activity patterns and assess their relationships with mood states and clinical characteristics in BD. The findings from this protocol will provide the preliminary data required to conduct studies to determine the timing relationships between locomotor activity, mood state, and clinical characteristics over time in BD, a fundamental knowledge gap in the field. The knowledge gained by conducting these protocols will allow for the design of actigraphy-based, illness monitoring paradigms that will allow for early intervention, thus, limiting the severity or onset of mood episodes and providing a step toward personalized medicine.

 Dost Öngür, MD, PhD
Dost Öngür, MD, PhD
Professor of Psychiatry,
Harvard Medical School and McLean Hospital
Xi Chen, PhD
Assistant Professor of Psychiatry,
Harvard Medical School and McLean Hospital
Lactate Dynamics During Working Memory in Bipolar Disorder
Changes in energy metabolism in brain cells may play an important role in bipolar disorder. These alterations could either directly affect brain functions or do so via effects on the transfer of information between neurons. Currently, MRI studies of brain metabolites and functions during the resting state may not fully address the cognitive impairments in bipolar disorder. There are few studies in vivo measuring bioenergetic and glutamatergic responses to brain activations during cognitive functions.
Lactate is an important intermediate of metabolic activity under glycolysis. Though originally thought of as a waste product, lactate is increasingly being studied as a supplemental fuel and signaling molecule. Lactate measurement using MR spectroscopy has been difficult because of its low signal and the overlapping of others. We recently developed a new technique termed HOPE to reliably measure lactate on 3T MRI scanners.
In the current study, we believe we will be the first to measure brain lactate dynamics in bipolar disorder in response to a working memory task. In the same scan that we measure lactate dynamics, we will also quantify the response of glutamate, an important neurotransmitter, to the task. Overall, we hope our study will provide more direct information on bioenergetic and neurotransmission abnormalities that may accompany impaired cognitive functions in bipolar disorder.
 Lauren Orefice, PhD
Lauren Orefice, PhD
Assistant Professor of Genetics and Molecular Biology,
Harvard Medical School and Mass. General Hospital
Understanding Oral Texture-Based Feeding Issues in Bipolar Disorder
Avoidant/restrictive food intake disorder, characterized by difficulties with specific food textures, is a common issue among individuals with bipolar disorder. This increased sensitivity to food textures significantly impacts the quality of life for those affected, leading to worse outcomes and increased risk for depression in people with bipolar disorder. Despite its prevalence, the cause of food texture difficulties in bipolar disorder remains unclear. By combining behavioral, anatomical, and electrophysiological techniques, we seek to uncover how gene mutations associated with bipolar disorder may affect the neural circuits responsible for processing food textures within the oral cavity and whether this affects feeding behaviors in mice. Importantly, the sensory pathways involved in oral texture perception are similar between mice and humans, allowing us to draw meaningful parallels to human conditions. Understanding the mechanisms that underlie oral texture sensitivity issues in bipolar disorder could pave the way for more targeted treatments and interventions to improve the lives of individuals affected by this challenging co-morbidity.
 Kerry Ressler, MD, PhD
Kerry Ressler, MD, PhD
Professor of Psychiatry,
Harvard Medical School and McLean Hospital
The Role of FoxP2 and Amygdala in Emotion and Bipolar Disorder
Bipolar disorder (BD) is characterized by alternating phases of increased appetitive drive (mania) and depression. Large genetic studies have begun to identify targets implicated in psychiatric disease, with intriguing findings in a gene called ‘Foxp2’ implicated in features of manic and depressive phases of BD. Foxp2 is expressed in a part of the brain called the amygdala, that modulates both positive and negative emotion. Preliminary findings from our lab suggest that Foxp2 is altered in its expression after negative emotional learning in mouse amygdala. This suggests a circuit-specific dynamic regulation of Foxp2 with emotional learning. Functionally, Foxp2 is a highly conserved gene, whose protein product regulates several known target genes implicated in development and neural signaling. Regulatory targets of Foxp2 include genes that are targets of lithium, widely used for BD treatment. Despite strong evidence for its involvement in psychiatry and data suggesting regulation by lithium, specific functional roles of Foxp2 in neural mechanisms of emotion regulation are unknown. This study will determine whether Foxp2 regulates specific components of positive and negative emotional circuits through signaling in amygdala, as a possible critical mechanism underlying aspects of BD.
2023-2024 Awards
 Pascal Kaeser, PhD
Pascal Kaeser, PhD
Professor of Neurobiology, Harvard Medical School
Mechanisms of Serotonin Neuromodulation in Bipolar Disorder
Serotonin is a modulatory signaling substance in the brain for the control of mood, perception, and reward. Drugs that operate on serotonin systems form a central pillar for the treatment of many brain disorders, including depression and bipolar disorder. Despite this clinical importance, there is a lack of precise understanding of how serotonin transmits signals between neurons. Our goal is to start addressing this knowledge gap. For conventional signal transmission in the brain, exquisitely organized molecular machinery controls the very high spatiotemporal signaling precision. Serotonin is thought to act on slower time scales and more promiscuously, but specific knowledge is largely absent. Building on recent studies in support of fast serotonin coding, we hypothesize that sophisticated machinery mediates rapid and synchronous serotonin release. Here, we define serotonin release machinery and regulatory mechanisms that control serotonin signaling. Overall, we expect to uncover signaling mechanisms that might support precise serotonin functions. The proposed work will help develop a fundamental understanding of a neuromodulatory system that is often targeted with drugs to treat brain disease.
 Mark Andermann, PhD
Mark Andermann, PhD
Professor of Medicine, Division of Endocrinology, Beth Israel Deaconess Medical Center
Do Serotonin, SSRIs and Lithium Boost Specific Interoceptive Channels in the Parabrachial Nucleus?
The insular cortex helps maintain health by sensing “interoceptive” signals from the body and using these to regulate emotions and guide behavior. Neuroimaging studies in patients with bipolar depression consistently show specific structural and functional impairments of the insular cortex. The depressive phase of bipolar disorder is often associated with impaired interoception, and with low levels of central serotonin. Drugs that boost serotonin levels in the brain, such as SSRIs, are used to treat bipolar depression. These drugs may act in part by restoring interoception. We hypothesize that serotonin enhances interoception by its actions on the lateral parabrachial nucleus, a key relay of bodily signals to the insular cortex. We will address this hypothesis by recording the activity of the same hundreds of lateral parabrachial nucleus or insular cortex neurons across weeks during multiple bodily manipulations as well as during delivery of lithium, SSRIs, and stimulation of serotonin neurons. We will then use 3D spatial transcriptomics to define the molecular identities of functionally characterized neurons. Together, these experiments will assess whether SSRIs and lithium augment interoceptive processing in insular cortex via serotonergic enhancement of sensory transmission in specific subtypes of brainstem neurons, thereby guiding new treatments for bipolar depression.

 Chinfei Chen, PhD
Chinfei Chen, PhD
Professor of Neurology, F.M. Kirby Neurobiology Center, Boston Children’s Hospital
Hisashi Umemori, PhD
Professor of Neurology, F.M. Kirby Neurobiology Center, Boston Children’s Hospital
Understanding How Information is Organized in the Thalamus That Regulates Mood and Cognition
There is growing evidence that communication between neurons carrying different lines of information is disrupted in many areas of the brain in bipolar disorder. One such area is the thalamus, a region located deep in the brain that acts much like a disc jockey with a sound mixer—the thalamus receives different channels of information which it then mixes and adjusts to produce a balanced output that can be fine-tuned based on the current situation or environment.
Here we propose to study how the different channels of information are organized in the limbic thalamus, the thalamic region that handles information related to emotion, memory, sensation and executive function. We will test the hypothesis that certain information channels are grouped together in compartments called glomeruli.To further understand the function of these compartments, we will monitor how communication between neurons changes when the glomerulus structure is disrupted.
The results of these studies will advance our understanding of the logic of how information channels are organized in limbic thalamus and provide insight into how disruption of this organization may lead to neuropsychiatric disorders such as bipolar disorder and psychosis.
 Maria Lehtinen, PhD
Maria Lehtinen, PhD
Professor of Pathology and Hannah C. Kinney, MD, Chair in Pediatric Pathology Research, Boston Children’s Hospital
Regulation of Brain Barrier Integrity and Inflammation in Bipolar Disorder
Neuroinflammation and associated brain damage are shared features of mood disorders including bipolar disorder. Although the underlying mechanisms remain unclear, available evidence suggests that compromised brain barrier integrity fosters neuroinflammation. We hypothesize that the choroid plexus, an important brain barrier between the blood and the cerebrospinal fluid (CSF), contributes to this process. Choroid plexus barrier disruption allows CSF entry of peripheral substances such as inflammatory mediators and environmental toxins, which have been shown to exacerbate psychiatric illness. Here, we have a rare opportunity to determine the degree to which the choroid plexus is disrupted in human bipolar disorder. In Aim 1, we will compare the choroid plexus transcriptome, inflammatory state, and barrier structure in bipolar disorder patients to controls in collaboration with Dr. Naguib Mechawar (Douglas Hospital Research Center, McGill University). In Aim 2, we will compare the protein composition of CSF samples from psychosis patients and controls in collaboration with Drs. Joseph Gonzalez and Mustafa Sahin (Boston Children’s Hospital). Discovery of key alterations in human samples taken together with parallel mechanistic studies in rodents will lay important groundwork for determining the diagnostic and therapeutic potential of the choroid plexus-CSF system in mental health conditions.
 Jessica M. Lipschitz, PhD
Jessica M. Lipschitz, PhD
Behavioral Scientist, Brigham and Women’s Hospital
Assistant Professor of Psychiatry, Harvard Medical School
Using Smartwatch Data to Classify Disease Trajectory and Predict Mood Episodes in Bipolar Disorder
The variation in the clinical presentation of bipolar disorder (BD) is one hypothesized reason for poor treatment outcomes. A precision medicine approach to treatment—in which treatment decisions are based on nuanced and objective measurement of each patient’s disease trajectory and then are adjusted for treatment response—may improve outcomes. At least two innovations are required for a precision medicine approach to BD treatment. The first is identifying, under the large umbrella of BD, clinically-meaningful subtypes that could inform treatment decisions. The second is developing remote tools to predict mood episodes (depression and mania/hypomania) between clinical appointments, prior to onset. Passive sensor data collected via smart devices offer an avenue for accomplishing both of these innovations. We propose to use passive sensors in smartwatches to track biobehavioral markers of BD over six months. We will apply machine learning methods to biobehavioral data to determine: whether clusters within these data meaningfully differentiate individuals on important clinical/functional features and whether mood episodes can be predicted before onset. The breakthrough targeted in the proposed study is to leverage commonplace technology to give clinicians tools to anticipate disease trajectory and respond to mood episodes that occur between routine appointments.

 Cagri Yuksel, MD
Cagri Yuksel, MD
Assistant Professor of Psychiatry, McLean Hospital
Dara Manoach, PhD
Professor of Psychology in the Department of Psychiatry, Mass. General Hospital
Association of Thalamus Biology with Sleep Spindles in Bipolar Disorder
Bipolar disorder is characterized by cognitive deficits, which are associated with poor psychosocial outcomes. However, current treatments are largely ineffective in addressing them. Therefore, there is an urgent need to identify new mechanisms underlying cognitive deficits, that can be targeted with novel treatments. Forming long-term memories is a fundamental cognitive faculty, essential for social and occupational functioning. A wealth of studies show that sleep supports “off-line” memory consolidation and sleep spindles have a central role in this process. Spindle initiation requires GABA-mediated inhibition of glutamatergic neurons in the thalamus. Therefore, thalamic GABA/glutamate balance is likely critical for spindle activity.
Recent studies suggest abnormal thalamus function in bipolar disorder. However, little is known about thalamic GABA-glutamate balance. In this study, using state-of-the-art in vivo neuroimaging methods, we will quantify thalamus GABA and Glu levels, in patients with bipolar disorder. In addition, overnight spindle activity and sleep-dependent memory consolidation will be examined. We hypothesize that thalamic GABA/glutamate ratio will be reduced in patients, and this reduction will be associated with spindle deficit and memory impairment. This study will be the first to probe a critical cognitive function in bipolar disorder, with its associated neurobiology at both molecular and functional levels.

 Jakob Hartmann, PhD
Jakob Hartmann, PhD
Assistant Professor of Psychiatry, Harvard Medical School
Associate Neuroscientist, McLean Hospital
Nikolaos P. Daskalakis, MD, PhD
Assistant Professor of Psychiatry, Harvard Medical School
Director, Neurogenomics and Translational Bioinformatics Laboratory, McLean Hospital
Associate Member, Stanley Center for Psychiatric Research, Broad Institute of MIT and Harvard
The Relevance of SKA2-Induced Glucocorticoid Dysregulation in Bipolar Disorder
Stress-related psychiatric disorders, including bipolar disorder (BD), are a global burden, but the molecular mechanisms are poorly understood. One of the primary control modules of the stress response in mammals is the hypothalamic-pituitary-adrenal (HPA) axis, which regulates the stress-induced release of glucocorticoids. Aberrant glucocorticoid release as a result of chronic stress or traumatic experiences can be damaging for the brain and increase the susceptibility to develop mental disorders. Therefore, disturbed activation or regulation of the body’s stress response through the HPA axis represents a common pathophysiological aspect of multiple stress-related diseases. Genes regulating HPA axis activity, including the glucocorticoid receptor (GR), have been linked to stress-related psychopathologies such as BD. The cell cycle gene SKA2 is a GR interaction partner, enhancing the receptor’s nuclear translocation in peripheral cells. Variants and DNA methylation within SKA2 have been associated with suicide risk and posttraumatic stress disorder. Moreover, lower SKA2 expression was reported in the prefrontal cortex of suicide victims. Our preliminary data identified SKA2 as a critical player in glucocorticoid signaling in the central nervous system, and provide evidence for its involvement in BD. However, the precise mechanism by which SKA2 regulates glucocorticoid signaling within neurons as well as its role in BD, remain largely unexplored. We aim to identify dysregulated gene networks in SKA2 knockout hiPSC-derived neurons by utilizing GR Chromatin Immunoprecipitation Sequencing (ChIP-Seq) and comparing the results to existing data from the PsychENCODE Consortium. Additionally, we will examine the effects of viral-mediated Ska2 depletion in the prefrontal cortex on stress resilience in mice. Increasing our understanding of GR-related transcriptional profiles that promote stress resilience vs susceptibility could inform the development of new treatment approaches for BD.

 Amit Anand, MD
Amit Anand, MD
Member of Faculty (Pending appointment as Full Professor), Department of Psychiatry,
Brigham and Women’s Hospital
Alexander Lin, PhD
Assistant Professor of Radiology, Brigham and Women’s Hospital
Monitoring the Effects of Lithium on Bipolar Brain Chemistry using Ultra High Field MR Spectroscopy
Lithium is a powerful treatment for patients who have bipolar disorder, but we don’t understand why it works well in some patients and not others. Studies have used magnetic resonance spectroscopy, a way of measuring chemicals in the brain to learn more about the effect of lithium however there are several problems with the earlier studies: 1) the studies were done on weaker MRI machines that don’t have enough power to measure chemicals at low levels. 2) the chemicals are measured at different times during treatment and may have missed the best times. 3) only certain areas of the brain were studied. We will address all of those issues by using an MRI machine that is twice as powerful and measure brain chemicals in patients before they start their lithium treatment, and then again at 2 weeks, 2 months, and 26 weeks so that we can see the effect at different times. Finally, we will develop a method to measure chemicals in the entire brain so we don’t miss an important area. We have brought together a team of experts to provide better treatments for bipolar patients. This study will provide valuable data for future funding for larger studies.
 Poornima Kumar, PhD
Poornima Kumar, PhD
Assistant Professor of Psychiatry, McLean Hospital
Building a Computational Model of Mood Instability in Bipolar Disorder
Bipolar disorder (BD) is characterized by (hypo)manic episodes interspersed with depressive episodes. However, clinical evidence shows that these episodes are often on a spectrum alongside with mood instability and mixed manic-depressive episodes. This ongoing mood instability and mixed states can lead to chronic functional impairment. Therefore, there is an urgent need to probe the underlying mechanisms of these mood variations in order to develop better treatments. A potential solution might be to adopt computational approaches to identify dissociable behavioral markers that explain the cause and maintenance of mood instability. Focusing on reward is a good starting point as abnormal reward processing has been shown during both manic and depressive episodes, however with mixed evidence. Therefore, we propose to test individuals with bipolar disorder longitudinally using an online administered reward learning battery that will offer us insights into the influence of mood variations on their behavior. We will use computational models to quantify these constructs that will help us identify behavioral biomarkers to understand the contribution of mood variations on this debilitating disorder, and potentially provide us initial clues about predictors for transition between relapse and recovery.
2022/2023 Awards

 Sandeep Robert Datta, MD, PhD
Sandeep Robert Datta, MD, PhD
Professor of Neurobiology, Harvard Medical School
Justin Baker, MD, PhD
Assistant Professor of Psychiatry, Harvard Medical School
Scientific Director, Institute for Technology in Psychiatry, McLean Hospital
Director of Functional Neuroimaging and Bioinformatics, Schizophrenia and Bipolar Disorder Research Program, McLean Hospital
Linking bipolar disorders to metabolism through machine learning-based behavioral analysis
Bipolar disorder (BD) causes mania and depression, both of which dramatically alter how patients expend energy, seek resources, and interact with the world. For both patients and healthy individuals, performing any action comes at a cost, which includes expenditure of energy as well as exposure to risk. For example, exploring an unknown environment to find new food sources expends precious energy stores and increases the likelihood of discovery by a predator. We hypothesize that there are neural signals and circuits that link the availability and current supply of energy to exploratory and risk-taking behaviors, and that these systems are disordered in BD. To test this hypothesis, we propose to use Motion Sequencing (MoSeq), an unsupervised behavioral discovery platform, to characterize the behavior of two mouse models of BD in which behavioral deficits are linked to metabolic changes (hyperthyroid and AKAP11 deleted mice), and also to characterize the behavior of humans with BD in whom endocrine and metabolic parameters are measured.
 Michael Do, PhD
Michael Do, PhD
Associate Professor of Neurology, Harvard Medical School
Research Associate, F.M. Kirby Neurobiology Center, Boston Children’s Hospital
A circadian control system for counterbalancing BD in early life
We are synchronized with the day/night cycle by an internal timekeeping mechanism, the circadian clock, which regulates patterns of gene expression and physiology in practically every tissue. Clock dysregulation is implicated in bipolar disorder. Because bipolar disorder is often diagnosed in adolescence, it is important to understand how the clock is regulated in early life. Light is the strongest regulator of the clock. Our laboratory will define how light regulates the clock from birth to adulthood, using a new experimental system that makes accessible the neural network that spans from eye to brain for this purpose. Our work will provide a foundation for understanding how this network may be compromised in bipolar disorder, and has the potential to guide the engineering of light-based therapies that impose regulation on the circadian clock of bipolar individuals to improve their health.
 Susan M. Dymecki, MD, PhD
Susan M. Dymecki, MD, PhD
Professor of Genetics, Harvard Medical School
Decoding the neural circuit logic underlying adaptation to seasonal photoperiods
Seasonal changes in day length (photoperiod) exacerbate the behavioral and physiological states that define bipolar disorder. We have discovered a dual serotonin-glutamate neuron type that may figure central for behavioral adaptation to seasonal photoperiods. This neuron type innervates brain centers involved in circadian rhythm and sleep/wake timing, segregates neurotransmitter differentially to these brain targets, and dramatically reorganizes this segregation in response to seasonal photoperiods, enabling robust behavioral adaptation. We have mapped brain inputs to these specialized dual serotonin-glutamate neurons, revealing sites likely critical for delivering daylight information. We will now test the importance of each of these inputs for behavioral adaptation. Results are expected to reveal novel brain circuits and cells that underlie adaptation to seasonal photoperiods of relevance to bipolar disorder and which may serve as novel therapeutic nodes.
 Rachelle Gaudet, PhD
Rachelle Gaudet, PhD
Professor of Molecular and Cellular Biology, Harvard University
How protocadherins wire the brain and how their dysfunction leads to miswiring in bipolar disorder
Synaptic network malformations are at the root of diseases like bipolar disorder, schizophrenia, depression, anxiety, and autism. Identity markers at the surface of neurons are essential for establishing functional neural network connections. We investigate a family of identity marker proteins, the clustered protocadherins, that are instrumental for self‐avoidance in brain development. Large assemblies of clustered protocadherins form when neurites from the same cell contact one another. These assemblies activate downstream signals that lead to self‐avoidance and ultimately ensure that a cell innervates the appropriate areas. Recent data on the interaction structure, affinity, and selectivity of clustered protocadherins suggest that dynamic factors contribute to assembly formation, but these dynamics have not yet been investigated. We will reconstitute an in vitro model of cell‐cell contacts and use time-lapse microscopy to answer questions like: How are clustered protocadherin assemblies organized? How do individual molecules move within and around assemblies? What changes in cell behavior occur after clustered protocadherin assemblies form? This work will reveal how clustered protocadherins participate in synaptic network development and identify perturbations that could contribute to neuropsychiatric disease or unlock potential therapeutic interventions.
Sam Gershman, PhD
Professor of Psychology, Harvard University
Towards a computational theory of bipolar disorder
Bipolar disorder is characterized by a menagerie of cognitive, sensory-motor, and physiological abnormalities. This project seeks to identify and formalize unifying principles underlying these abnormalities. The starting point is a computational model of resource allocation based on dopamine signals. This model has previously been used to explain the diverse roles of dopamine in regulating cognition and perception. This project will extend the model to incorporate the role of dopamine in energy regulation, thereby capturing the critical role of this process in healthy brain function, and its breakdown in bipolar disorder. To validate this model, we will apply it to data from healthy humans, bipolar patients, and mice with hyperthyroidism (a rodent model of energetic dysfunction in bipolar disorder). We hypothesize that seemingly disparate aspects of bipolar disorder can be explained in a unified way.
 Jonathan Lipton, MD, PhD
Jonathan Lipton, MD, PhD
Assistant Professor of Neurology, Harvard Medical School
Faculty, Kirby Center, Boston Children’s Hospital
Prion-like properties of CLOCK as biophysical and synaptic capacitors for mania
Disruption of circadian rhythms is a nearly ubiquitous feature of bipolar disorder but the mechanisms of this association remain obscure. In this proposal we test the hypothesis that flexibility in the structure and function of the core circadian protein CLOCK provides essential resilience of circadian rhythms to perturbation. Understanding these mechanisms could offer previously unappreciated targets for treating bipolar disorder.
 Dragana Rogulja, PhD
Dragana Rogulja, PhD
Associate Professor in Neurobiology, Harvard Medical School
Understanding arousal problems associated with bipolar disorder
Both the manic and depressive phase of bipolar disorder are associated with sleep disturbances. During mania the patients are highly aroused and sleep less, while during depression they can spend much of their time in a hypoaroused state, sleeping. They are often unable to reach the deepest stages of sleep and feel unrestored. It is possible that sleep disturbances and bipolar disorder share a common origin, and at the very least it is evident that sleep problems exacerbate the symptoms of mania and depression. We want to understand the connection between sleep and bipolar disorder, with the ultimate goal of improving sleep quality—which we think could ameliorate some of the health problems associated with bipolar disorder.
 Bernardo Sabatini, MD, PhD
Bernardo Sabatini, MD, PhD
Alice and Rodman W. Moorhead III Professor of Neurobiology, Harvard Medical School
Co-Director, Kempner Institute for the Study of Natural and Artificial Intelligence at Harvard University
Perturbed kinase signaling arising from mutations in the bipolar disorder risk gene AKAP11
Recent studies on genetic contributions to bipolar disorder have identified rare mutations to the gene Akap11 as strongly contributing to disease risk in affected individuals. Akap11 is known to encode a protein that interacts with protein kinase A (PKA), a central signaling molecule in neurons that controls neuronal excitability, synaptic plasticity, and gene transcription. The role of Akap11 in regulating PKA and its role in neurons are otherwise unknown. We propose to study changes in PKA signaling in mice carrying mutations to Akap11 using genetically-encoded biochemical sensors that grant us high temporal resolution measurements on PKA activation at subcellular scales. We will identify in which cells PKA activation is altered by Akap11 mutations and any changes in the subcellular localization of PKA. Previous work from our lab has also shown that PKA signaling in the striatum is essential for reward processing and reinforcement-based learning, which are known to be altered in psychiatric diseases such as bipolar disorder. We will therefor also test how behavior is altered in a reinforcement learning task in Akap11 mutant mice, and related behavioral changes to alterations in PKA activity. These experiments will provide a framework for how a significant bipolar disorder risk gene alters brain signaling upon which future treatments may be developed and tested.
 Martin H. Teicher, MD, PhD
Martin H. Teicher, MD, PhD
Director, Developmental Biopsychiatry Research Program, McLean Hospital
Associate Professor of Psychiatry, Harvard Medical School
Is there a subtype of bipolar disorder in which the major physiological problem is a disturbance in temperature regulation?
Bipolar disorder is not a single disease but a constellation of diverse problems in brain function that give rise to overlapping sets of symptoms. Substantial progress will be made by identifying biologically specific subtypes. We propose that there is a specific bipolar subtype characterized by insensitivity to cool temperatures and an impaired ability to thermoregulate through heat dissipation, which results in mood swings, nightmares, sleep disturbances and weather sensitivity. Our preliminary data suggests that 15% of adults with bipolar disorder may have significant problems with temperature regulation. Further, bipolar symptoms often emerge at an early age in these individuals, and they may fail to benefit from antipsychotic drugs and most mood stabilizers. Conversely, they may respond favorably to ketamine, which facilitates heat dissipation. We propose to compare adults with bipolar-I disorder with symptoms of temperature dysregulation to bipolar-I individuals without these symptoms to test the hypothesis that these two groups differ physiologically in temperature sensitivity, temperature regulation during sleep and ability to dissipate heat to prevent brain temperature from rising excessively during heat stress. Verifying distinct physiological difference will lend credence to the possibility of a temperature-dysregulated subtype with a novel underlying molecular biology and unique therapeutic requirements.
2021/2022 Awards
 Todd Anthony
Todd Anthony
Assistant Professor of Psychiatry and Neurology
Harvard Medical School and Boston Children’s Hospital
Mechanisms underlying co-morbidity of mood and sleep disruptions in bipolar disorder
Bipolar Disorder (BD) is typically diagnosed based on sustained alterations of mood, but sleep disruptions are a core symptom of the illness that affect virtually all people with BD. Moreover, sleep impairments in BD patients are thought to contribute to the disease process itself and can be present even during periods when mood states are normal. However, we currently lack a basic understanding of how sleep dysfunction can influence mood. Our group is pursuing a promising approach to this problem by focusing on a single neuronal population that we have found controls both sleep and mood states in mice. In this project, we will determine how activity of these neurons normally fluctuates during sleep-wake states, and how such activity patterns change following stressful experiences that persistently disrupt both sleep and mood. Further, we will test whether particular activity patterns are perturbed when a gene implicated in BD is disrupted in these neurons. Together, these studies will provide fundamental insight into the neural mechanisms that underlie the close relationship between mood and sleep, and may suggest new approaches that could be pursued to improve treatments for people with BD.
Katherine E Burdick
Associate Professor of Psychiatry
Harvard Medical School and Brigham and Women’s Hospital
Immune-related treatment targets in bipolar disorder
Bipolar disorder (BD) is highly heterogeneous. Some people with this condition function very well, whilst others struggle to hold down a job. Identifying the modifiable risk factors that contribute to poor outcomes provides treatment targets to optimize quality of life. We have identified several clinical risk factors for poor outcomes, (e.g., high recurrence rate, sleep disruption, childhood trauma, and cognitive impairment). The biological risk factors for poor outcome are unknown; however, evidence suggests that immune dysfunction plays a key role. Acute mood episodes trigger inflammation, which is believed to accumulate with illness recurrence and contribute to changes in brain structure and function, making this a potential target for intervention.
The immune system is a complex network that acts in concert to maintain homeostasis; perturbations in any of its individual components can result in a cascade of deleterious effects. Comprehensive studies are needed to identify specific therapeutic targets. In this study, we will assay three levels of immune function: a) innate immunity [plasma-based cytokines (e.g. TNFα; IL-6), b) adaptive immunity [mononuclear cell frequencies (e.g. CD4; CD8), intracellular cytokine expression], and c) thyroid hormone activity (e.g. TSH, T3, T4, thyroid auto-antibodies) to identify specific abnormalities in individuals with BD that can be targeted to improve outcomes.
 Ryan Doan
Ryan Doan
Assistant Professor of Pediatrics
Harvard Medical School and Boston Children’s Hospital
Noncoding genetics of bipolar disorder
The phenotypic complexity of bipolar disorder and increased prevalence of co-existing diagnoses result in a strikingly diverse genetic etiology, leaving most of the genetic contribution unexplained. Recent data, including our own, suggest that much of the missing genetic etiology of many neuropsychiatric disorders lies within noncoding regions including gene promoters and regulatory elements. Therefore, it is likely that abnormal gene expression, due to underlying genetic mutations, contribute to the manifestation of bipolar disorder. We will perform DNA sequencing in families with bipolar disorder to systematically assess the role of mutational disruption of gene expression. The functional consequences of identified candidate mutations, genes, and genomic elements will be assessed through a combination of computational predictions and functional modeling. We aim to 1] assess the role of regulatory mutations in bipolar disorder, 2] develop improved guidelines for interpreting noncoding mutations and to 3] advance the understanding of the functional roles of noncoding regions. The completion of our aims will lead to novel insights into the genetic underpinnings of bipolar disorder and will expand the availability of clinical genetic diagnoses for families.
 Susan Dymecki
Susan Dymecki
Professor of Genetics
Harvard Medical School
A specialized brainstem cell type may link mood disorders with seasonal changes in day length
Seasonal changes in day length (photoperiod) exacerbate the behavioral and physiological states that define bipolar disorder. Mania is most prevalent during spring/summer, while episodes of depressive disorder occur most frequently in the fall/winter. Despite bipolar disorder afflicting ~3% of the population worldwide – a substantial unmet medical need – the underlying neural circuits and causative dysfunctions are just beginning to be understood. Treatment options are limited, often ineffective, and not without major side effects. Here we investigate in mouse models the involvement of a distinct group of brain neurons that may underlie behavioral adaptations to seasonal photoperiod changes. We are motivated by the potential of these neurons and associated brain circuits to serve, by extension in humans, as a possible therapeutic target for novel treatments for bipolar disorder.
 Rakesh Karmacharya
Rakesh Karmacharya
Associate Professor of Psychiatry
Harvard Medical School and Massachusetts General Hospital
Neural network activity in patient-derived brain organoids in bipolar disorder
Human studies show specific differences in oscillatory brain dynamics in bipolar disorder. Differences in these oscillations are thought to underlie cognitive deficits. Moreover, mood stabilizers used to treat bipolar disorder, such as lithium and valproate, have been shown to affect brain oscillatory activity. In order to develop experimental models for interrogating neural network activity relevant to bipolar disorder, we have generated induced pluripotent stem cells from bipolar disorder patients. The stem cells are used to grow patient-specific brain organoids in the laboratory. These brain organoids show regular oscillatory activity and bursts of spontaneous network-synchronized spikes when they are nine months old. Our preliminary experiments show abnormal response to electrical stimulation and depolarization in bipolar disorder brain organoids. We will undertake comprehensive functional characterization of patient-derived brain organoids to collect data on periodic and oscillatory events under normal growth conditions and in the setting of specific perturbations, in order to delineate differences in neural network activity in bipolar disorder organoids. In addition, we will examine the effects of a set of mood stabilizers in clinical use on neural network properties in the brain organoids.
 Jonathan Lipton
Jonathan Lipton
Assistant Professor of Neurology
Harvard Medical School and Boston Children’s Hospital
Exploring local circadian control of presynaptic function as a therapeutic target in bipolar disorder
The circadian timekeeping system is a biological clock that synchronizes our sleep/wake behavior, cognitive function, and cellular physiology with the earth’s light/dark cycle. The disruption of sleep and circadian rhythms are among the most common features of Bipolar disorder (BD) but the neurobiology that links circadian clocks to synaptic function remains unknown. We have discovered that a core molecule in the circadian clock is localized to mammalian synapses where it exerts a crucial role in organizing presynaptic function in a manner that implicates serotonin, a neurotransmitter critical to the treatment options for BD. In this project, we will investigate how serotonin regulates the circadian clock in synapses and establish how circadian control of presynaptic function regulates sleep architecture and homeostasis. Our experiments could establish a novel paradigm for local circadian control in synapses and yield fundamental principles that link circadian clocks and presynaptic plasticity to the pathobiology of BD.

 Pamela Mahon
Pamela Mahon
Assistant Professor of Psychiatry
Harvard Medical School and Brigham and Women’s Hospital
Alexander Lin
Assistant Professor of Radiology
Harvard Medical School and Brigham and Women’s Hospital
Dynamic modulation of glutamate and GABA during an emotional linguistic task in bipolar disorder
A core deficit in bipolar disorder is difficulty in emotion regulation, with abnormal response to emotional stimuli observed at the level of both behavior and brain circuits. Dysfunction in glutamatergic (primary excitatory) and GABAergic (primary inhibitory) metabolism in the brain may give rise to the deficits in emotion regulation observed in bipolar disorder. At rest, brain levels of glutamate and GABA are different in emotion regulation network regions in people with a mood disorder, although not consistently. This is likely because resting levels capture information at a single time point and are not sufficient to distinguish dynamic modulation of glutamate and GABA that may occur in the brain during emotion regulation. In a collaboration between our labs, we propose to optimize a new functional magnetic resonance spectroscopy protocol to examine real-time changes in glutamate and GABA levels in the brain during an emotional linguistic (word-based) response inhibition task in participants with and without bipolar disorder. Our project will deepen understanding of the specific roles of glutamatergic and GABAergic functioning in emotion regulation networks, with future potential to inform the development of novel pharmacological and neurostimulation treatment interventions.
 Naoshige Uchida
Naoshige Uchida
Professor of Molecular and Cellular Biology
Harvard University
Balance between pessimism and optimism: using a novel theoretical framework to study bipolar and major depressive disorders
Bipolar disorder and major depressive disorder are characterized by abnormal mood and abnormal predictions of future events. Previous studies have indicated that mood as well as learning to predict future outcomes depends not on the absolute goodness of outcomes, but rather on reward prediction error: the discrepancy between actual and expected outcomes. Dopamine neurons in the midbrain are known to signal reward prediction errors, and dopamine has been implicated in these disorders. However, whether and how altered dopamine signals lead to abnormal reward predictions and abnormal mood remain unclear. In this study, we will test how the activity of dopamine neurons, as well as their upstream neurons in the lateral habenula, are altered by manipulations that induce manic or depressive states in mice, and whether their altered activities are reversed by lithium or the anti-depressant, ketamine. To understand how altered dopamine signals may lead to altered reward predictions, we will use a novel theoretical framework developed in the field of artificial intelligence — distributional reinforcement learning. We hypothesize that manipulations that cause depressive or manic states will alter the ensemble activity patterns of dopamine neurons, in a manner consistent with pessimistic or optimistic biases in reward prediction.
 Charles Weitz
Charles Weitz
Robert Henry Pfeiffer Professor of Neurobiology
Harvard Medical School
A three-dimensional picture of the body’s circadian clock machinery
Circadian clocks are biological machines in our cells that measure time on a 24-hour basis. Circadian clocks govern a myriad of daily rhythms, such as the sleep-wake cycle and daily cycles in mood and metabolism. Circadian clocks coordinate processes all over the body and set them to the optimal time of day.
Disturbances of circadian rhythms are a hallmark of bipolar disorder, which some investigators now consider a disease of impaired circadian clock function. Despite the rich evidence for this connection, there is no explanation for circadian defects in bipolar disorder. Our understanding of the clock is simply too crude to supply useful ideas.
Work from our laboratory shows that the circadian clock proteins act as part of a large multi-protein machine, not alone or in pairs a previously believed. We have no idea how this imposing machine is built or how it functions. We aim to produce a detailed three-dimensional picture of this circadian clock machine using cryo-electron microscopy, a revolutionary technique for visualizing protein structure.
A successful outcome would be far-reaching. It would dramatically advance our picture of the circadian clock, potentially revolutionizing efforts to understand what might go wrong with the circadian clock in bipolar disorder.
 Tracy Young-Pearse
Tracy Young-Pearse
Associate Professor of Neurology,
Harvard Medical School and Brigham and Women’s Hospital
Elucidating the function of the bipolar disorder risk gene POU3F2 in neurons
Neuropsychiatric disorders, such as schizophrenia and bipolar disorder, present a major societal health burden and have been shown to be heritable and polygenic, including a complex interplay between rare, highly penetrant variants and common variants with small effect sizes. While improved sample size of genome-wide association studies has increased the number of loci associated with neuropsychiatric disease, the molecular mechanisms underlying the disease-related variants is unknown. Here, we examine the role of the gene POU3F2 in human neurons and in the rodent brain, a gene identified in these human genetic studies to be linked to bipolar disorder. Our preliminary data suggest that reductions in POU3F2 protein levels in human neural cells results in the upregulation of inhibitors of the WNT signaling pathway. Interestingly, the Wnt pathway has been previously linked to neuropsychiatric disease risk and progression. Using both human induced pluripotent stem cell technology and conditional knock out technology in mice, we will interrogate the function of POU3F2 in both neural progenitor cells and adult neurons.
2020-2021 Awards
 Michael Tri H. Do
Michael Tri H. DoAssociate Professor of Neurology
Harvard Medical School & Boston Children’s Hospital
Connecting the circadian clock, light, and bipolar disorder
The earth’s rotation drives profound changes in our environment. Practically every tissue of the body is synchronized to this rhythm by an internal timekeeping mechanism, the circadian clock. Desynchronization impairs mood, cognition, and physiology—commonly experienced in shift work and jet lag. These impairments are reversed as the clock is realigned to the solar day, a process that depends critically on proper exposure to light. A deeper failure of the clock can result in bipolar disorder, which is exacerbated or alleviated by light. By understanding how light regulates the clock, we aim to provide new insights into bipolar disorder and its treatment. Supported by a Bipolar Seed Grant, we have developed a method to access the pathway that connects the eye to the master clock in the brain. We will now define how information flows through this pathway into clock circuitry. In the longer term, we will ask if this pathway is altered in bipolar disorder and can be manipulated for therapeutic purposes. We expect to provide knowledge of how physiology is tuned to environmental cycles, and of how tuning mechanisms can be leveraged to improve health.
 Lisa Goodrich
Lisa Goodrich
Professor of Neurobiology
Harvard Medical School
FAT cadherins and the neurobiology of bipolar disorder
Although bipolar disorder has a clear genetic component, we do not understand how specific mutations act at the cellular level to alter nervous system function. In this project, we will investigate the possibility that some bipolar disorder-associated mutations cause fine-grained changes in the pattern of connections among neurons, which are called synapses. Our work is inspired by the identification of the atypical cadherin FAT as a susceptibility gene. FAT cadherins allow cells to communicate with each other and therefore assume the correct shape and position needed for the whole tissue to function. Although FAT is enormous, mutations associated with bipolar disease cluster together in one region of the protein. In characterizing the FAT-related protein Fat3 in mice, we discovered that analogous mutations cause neurons to form extra synapses. Additionally, we identified multiple interacting proteins that appear to participate in an evolutionarily conserved FAT pathway. We will further define this pathway and its role in the nervous system by studying Fat3 in the retina, where even subtle changes in circuit organization are readily detected. With a better grasp on the FAT pathway and its effects on neurons, we can generate new, testable hypotheses about how synapses are affected in bipolar disorder.
 Maria Lehtinen
Maria Lehtinen
Associate Professor of Pathology
Harvard Medical School & Boston Children’s Hospital
Elucidating the role of serotonergic signaling at the choroid plexus in bipolar disorder
Therapeutic options for bipolar disorder are suboptimal. Combination therapies that include supplementing lithium, a mainstay of bipolar disorder therapy, with commonly used anti-depressants (e.g. selective serotonin reuptake inhibitors) have proven promising for treatment-resistant forms of depression. However, the mechanisms of therapeutic action remain poorly understood. While serotonin metabolites are used as biomarkers of mental health, individuals with major depression can also have reduced levels of cerebrospinal fluid (CSF) Transthyretin (TTR). TTR represents the most highly expressed signature gene of the choroid plexus, a sheet of epithelial cells that produces CSF and health-promoting factors for the brain. Notably, the TTR locus is implicated in inherited bipolar disorder. In addition, Ttr-deficient mice show anti-depressant-like behaviors, and lithium alters choroid plexus-Ttr expression in rats. New therapies targeting serotonin receptors, some of which are highly expressed in choroid plexus, have been developed for psychiatric disease. Together, these findings suggest that the choroid plexus represents an unrecognized target site of bipolar disorder therapies. In Year 1, we discovered that certain serotonin agonists drive vesicular exocytosis and can produce large-scale, ‘apocrine’ secretion of choroid plexus epithelial cell contents into CSF. Now, with our Year 2 funding, we plan to use chronic imaging of choroid plexus to test whether these forms of secretion are modulated by SSRIs and by lithium delivery, and the effects on levels of fluorescently tagged TTR in the CSF. Our approach will open avenues for developing future therapies that harness the choroid plexus-CSF system for the treatment of bipolar disorder.
 Venkatesh Murthy
Venkatesh Murthy
Raymond Leo Erikson Life Sciences Professor of Molecular & Cellular Biology
Harvard University
Neuronal mechanisms of altered reward sensitivity in bipolar disorder
Bipolar disorder is a complex behavioral disorder characterized by bidirectional changes in motivation and reward responsivity. One recent model of bipolar disorder is hypersensitivity to reward in the networks linking prefrontal cortex to ventral striatum and amygdala. In addition to elevated responses to rewarding stimuli in these networks in bipolar patients, there is also evidence that there is altered connectivity between them, and overall increased striatal volume. We propose to study reward sensitivity directly with the use of rewarding and aversive odors in the olfactory tubercle region of ventral striatum, which receives direct odor information and dense dopaminergic input. In addition to its involvement in odor processing, the olfactory tubercle is known to powerfully modulate motivation and addictive behavior. We suggest that olfactory tubercle may be involved in bipolar disorder not only on the basis of its documented key role in motivation, but also due to findings that odor sensitivity is modulated as a function of mental state in bipolar patients. We will first characterize neuronal activity and dopaminergic activity in the olfactory tubercle in response to odors predicting rewarding or aversive outcomes with the use of 2-photon imaging of calcium activity in the cell bodies of identified subtypes of neurons, as well as dopaminergic axons. We will then correlate this reward sensitivity to overall optimistic or pessimistic states of the animal. Finally, we will investigate how pharmacological drugs used in the treatment of bipolar disorder alter reward responsivity in these neuronal populations.
 Olivier Pourquie
Olivier Pourquie
Frank Burr Mallory Professor of Pathology
Harvard Medical School & Brigham and Women’s Hospital
Understanding developmental origin of bipolar disorder and brain laterality
A striking feature of bipolar disorder and other neurological diseases such as schizophrenia or autism is their association with brain symmetry defects, together with increased numbers of left-handed and mixed handedness individuals among patients. While the nervous system is organized in a bilaterally symmetrical fashion, in humans, the brain shows clear left-right asymmetries both morphologically and functionally. For instance, in most people, the language centers are found in the left hemisphere, which also controls the dominant right hand. Although this asymmetry is a prominent feature of the brain, how it is established in this otherwise symmetrical organ is poorly understood. We have recently identified the first mouse mutant showing a handedness and brain laterality phenotype. In wild-type mice, there is no preferred hand usage at the population level. In contrast, we observed a skewed preference toward right-hand usage (80%) as well as subtle brain asymmetry defects in heterozygous mutants for the retinoic acid (RA) coactivator Rere. We propose to examine the role of the Rere-dependent RA pathway in establishing brain asymmetry and in the development of functional asymmetries such as handedness. We expect these studies to provide a basis for understanding the symmetry defects observed in patients with bipolar disorder.
 Vetrivelan Ramalingam
Vetrivelan Ramalingam
Assistant Professor of Neurology
Harvard Medical School & Beth Israel Deaconess Medical Center
Bipolar disorder and sleep-wake abnormalities
Bipolar disorder (BD), characterized by alternating episodes of mania and depression, affects about 3% U.S adult population. In addition to the mood and other behavioral changes, manic and depressive episodes in BD are accompanied by specific alterations in sleep behavior. For example, substantially higher amounts of rapid eye movement (REM) sleep and REM sleep occurring very soon after sleep onset are hallmark features of depressive episodes. In contrast, the need for sleep is greatly reduced during manic episodes. The REM sleep changes are observed even at the preclinical stage, and abnormal expression of REM sleep is even considered to be a reliable marker to predict BD. Lithium and antidepressants used in the BD treatment decrease or abolish REM sleep; Conversely, REM sleep deprivation effectively reverses depressive symptoms, induces mania, and worsens pre-existing manic BD symptoms in animals and humans. This project is aimed to understand the neural basis of the bidirectional relationship between REM sleep and bipolar disorder using animal models. The project outcomes are expected to identify new drug targets to improve various symptoms of BD in addition to advancing our understanding on the BD pathophysiology.
 W. Brad Ruzicka
W. Brad Ruzicka
Assistant Professor of Psychiatry
Harvard Medical School & McLean Hospital
Single-cell RNA splice variants in bipolar disorder
Alternative splicing of RNA transcripts is a basic and widespread mechanism that greatly increases biological complexity by allowing a single gene to encode multiple functionally distinct protein products. In bipolar disorder RNA splicing patterns show variability of greater effect size, disease specificity, and disease-associated genetic enrichment than overall gene expression, but methods used most often to investigate bipolar disorder pathology are blind to this mechanism. Studies that do investigate this highly cell-type specific mechanism often focus on small lists of target genes, and interrogate whole-tissue homogenates—diminishing their sensitivity and making them unable determine the cell-type or circuit-location specificity of their findings.
Under this award we will measure RNA splicing genome-wide at multiple anatomic locations within postmortem human hippocampus tissue from subjects with bipolar disorder and control individuals. In these same tissue samples, we will also measure cell-type specific gene expression profiles with single-nucleus RNA sequencing. Computational integration of these two RNA expression measurements will determine the cell-types impacted by identified RNA isoform expression changes. Investigation of this understudied mechanism genome-wide at specific sites within the complex cellular architecture of the human brain will generate new insights into bipolar disorder pathophysiology and identify novel targets for further study and potential therapeutic intervention.
 Leah Somerville
Leah Somerville
Professor of Psychology
Harvard University
Development of brain networks underlying executive functioning as a lens into cognitive deficits of bipolar disorder
Executive functions such as working memory, inhibitory control, and cognitive flexibility regulate goal-directed behavior, and continue to develop through childhood and adolescence. Deficits in executive functions represent a core symptom category of bipolar disorder, which may stem from the aberrant development of regulatory brain networks during adolescence. Therefore, understanding the mechanisms and predictors of bipolar disorder risk requires taking a developmental perspective. Our research will use nonininvasive human brain imaging from a large national study of neurodevelopment in individuals aged 5-21 years, paired with comprehensive cognitive testing, to characterize patterns of brain connectivity supporting the development of different components of executive ability and to identify predictors of individual variability in this development. This work will provide a foundation for translational research focused on the mechanisms underlying cognitive deficits in psychopathologies such as bipolar disorder.

 Andrew Nierenberg
Andrew Nierenberg
Professor of Psychiatry
Harvard Medical School & Massachusetts General Hospital
Paola Arlotta
Golub Family Professor of Stem Cell and Regenerative Biology
Harvard University
Growing brain organoids from individuals with bipolar disorder to understand the biology of response to treatment
Bipolar disorder (BPD) is a lifelong mood disorder whose treatment outcomes are variable and unpredictable, with many people recovering from acute episodes and depression, but many others experiencing frequent relapses or continuous mood symptoms. While many studies have begun to define the genetics of BPD, we still have a limited understanding of the cellular and molecular defects of the disease and why some people are responsive to treatment while others are not. Here we will leverage the large patient population at the MGH bipolar clinic and the ability to generate patient-derived 3D human brain organoids to begin work aimed at identifying features associated with treatment outcomes in BPD. We will select a small number of patients at the opposite spectrum of the response to treatment. We will then generate brain organoids from patient-derived adult inducible pluripotent stem cells, and apply high-throughput molecular assays to determine phenotypic differences among these two groups. Such differences will inform on biological processes and mechanisms of resistance to treatment for further validation in large cohorts of patients. While exploratory in nature, the work will provide an experimental platform to inform future directions of research towards better patient-tailored therapeutic opportunities.
2019-2020 Awards
 Adam Cohen
Adam Cohen
Professor of Chemistry & Chemical Biology and Physics, Harvard University
Impact of estrous cycle on neocortical dynamics in bipolar disorder
Bipolar disorder (BD) generally afflicts men and women at similar rates, but women are more likely to be diagnosed with BD Type II, a form in which patients transition more frequently between manic and depressive episodes. Clinical studies suggest that the menstrual cycle contributes to this rapid cycling. Female patients with BD are also more susceptible to relapse during perinatal periods. These findings suggest that hormonal changes might modulate the neural circuit dysfunction associated with BD in women. However, little is known about the impact of sex hormones on cortical circuit function, either in health or in disease. Understanding this impact will yield mechanistic insight into BD in women, and potentially in men also.
We propose to study how sex hormones modulate the balance of excitation and inhibition in cortical neurons, and how this modulation affects local circuit dynamics and ultimately behavior. We will perform these measurements using an in vivo all-optical electrophysiology platform we recently developed. By combining single-cell optogenetic stimulation with voltage imaging, this platform enables measurement of neuronal excitability and of identified synaptic connections across days and weeks in behaving animals.
 Fei Du
Fei Du
Assistant Professor of Psychiatry, Harvard Medical School & McLean Hospital
Dost Öngür
William P. and Henry B. Test Professor of Psychiatry, Harvard Medical School & McLean Hospital
Correcting brain energy metabolism abnormalities in first-episode bipolar disorder using nicotinamide riboside
A converging line of evidence indicates abnormalities in brain energy metabolism in bipolar disorder, however, currently there are no available treatments that directly target these impairments. Neurons primarily rely on oxidative metabolism to produce energy and the ratio of the oxidized and reduced nicotinamide adenine dinucleotide is a key regulator of this process. Reduction in this redox ratio inhibits glucose metabolism and increases oxidative stress.
Using state of the art neuroimaging methods, we recently showed a substantial decrease in redox ratio in first episode bipolar disorder. Similar reductions have been reported in other disorders with well-documented energetic impairments, such as diabetes.
Nicotinamide riboside, a newly discovered molecule, is a potent stimulator of the oxidized form of nicotinamide adenine dinucleotide. Consistent with this effect, a fast-expanding literature shows that it dramatically enhances glucose tolerance and mitochondrial activity. In animal models, nicotinamide riboside improves neuroinflammation, hippocampal plasticity and cognitive functions. However, no study to date has tested its effects in human brain. In this study, we propose to administer nicotinamide riboside to patients with first episode bipolar disorder and measure its effect on brain redox ratio, utilizing neuroimaging methods. We hypothesize that, nicotinamide riboside will correct brain redox ratio in patients. If these results hold, they will open the way for futures studies that will test the effectiveness of nicotinamide riboside on improving other aspects of brain energy metabolism, structural deficits and cognitive functions in bipolar disorder.
 Corey Harwell
Corey Harwell
Assistant Professor of Neurobiology, Harvard Medical School
Dissecting the development and diversity of septal nuclei circuits implicated in bipolar disorder
Septal nuclei in the basal forebrain have critical roles in regulating emotional states including fear, anxiety, and aggression. Dysfunction of septal neurons is thought to play a significant role in the pathophysiology of a variety of psychiatric disorders including schizophrenia, bipolar disorder and depression. Very little is known about the development and diversity of neurons that contribute to septal circuit function. Our lab will utilize high throughput single cell sequencing and lineage tracing to understand the cellular and molecular pathways required for the assembly of distinct septal neuron circuits. Our work will provide a framework for understanding the functional diversity of neuron types in the septum and the genetic programs that guide this diversification and could lead to the identification of new therapeutic targets or strategies in the treatment of bipolar disorder.
 Emma Knowles
Emma Knowles
Member of the Faculty, Harvard Medical School & Boston Children’s Hospital
Examining the impact of voltage-gated calcium channel genes on risk for bipolar disorder in
early-onset bipolar trios
Large-scale genome-wide association studies have discovered robust associations between common genetic variation within voltage-gated calcium-channel genes and risk for bipolar disorder. This discovery has improved our understanding of the broad molecular underpinnings of bipolar disorder, yet the specific mechanisms that drive this association remain unclear. Valuable mechanistic insights may be provided by identifying rare functional genetic variations of large effect within the narrow search space of voltage-gated calcium channel genes and their associated gene networks.
Previous studies on the genetics of bipolar disorder used adult samples. This makes sense because the modal age of onset is between late adolescence and young adulthood. However, bipolar disorder can occur earlier—in early adolescence or even childhood—in some individuals. Individuals with early-onset bipolar disorder are particularly valuable to genetic research because they may be subject to a greater genetic load than individuals with typical-onset forms of the illness.
We will evaluate inheritance patterns of rare genetic variants in VGCC genes and gene networks in child-affected bipolar trios and measure the strength of their relationship with specific symptoms of bipolar disorder including (hypo)mania. This data will improve understanding of the mechanistic role of calcium dysregulation in bipolar disorder.
 Maria Lehtinen
Maria Lehtinen
Hannah C. Kinney MD, Chair in Pediatric Pathology Research, Boston Children’s Hospital; Associate Professor of Pathology, Harvard Medical School
Elucidating the role of serotonergic signaling at the choroid plexus in bipolar disorder
Therapeutic options for bipolar disorder are suboptimal. Combination therapies that include supplementing lithium, a mainstay of bipolar disorder therapy, with commonly used anti-depressants (e.g. selective serotonin reuptake inhibitors) have proven promising for treatment-resistant forms of depression. However, the mechanisms of therapeutic action remain poorly understood. While serotonin metabolites are used as biomarkers of mental health, individuals with major depression can also have reduced levels of cerebrospinal fluid (CSF) Transthyretin (TTR).
TTR represents the most highly expressed signature gene of the choroid plexus, a sheet of epithelial cells that produces CSF and health-promoting factors for the brain. Notably, the TTR locus is implicated in inherited bipolar disorder. In addition, Ttr-deficient mice show anti-depressant-like behaviors, and lithium alters choroid plexus-Ttr expression in rats. New therapies targeting serotonin receptors, some of which are highly expressed in choroid plexus, have been developed for psychiatric disease. Together, these findings suggest that the choroid plexus represents an unrecognized target site of bipolar disorder therapies. We will test if combination therapies used for the treatment of bipolar disorder regulate choroid plexus functions. Our approach will open avenues for developing future therapies that harness the choroid plexus-CSF system for the treatment of bipolar disorder.
 Bernardo Sabatini
Bernardo Sabatini
Alice and Rodman W. Moorhead III Professor of Neurobiology, Harvard Medical School
Elucidating the role of distinct cell types of the dorsal raphe nucleus in bipolar disorder
The serotonergic system has been implicated in the pathogenesis of mood disorders, yet little is known about the mechanisms by which dysfunction of serotonergic neurons causes behavioral deficits. Although reduced serotonin signaling has been associated with bipolar disorder, there is a paradoxical involvement of serotonin in both depressive and manic behaviors.
The dorsal raphe nucleus houses the majority of serotonergic neurons in the brain, and also contains other cell types that interact locally with serotonergic neurons. Findings from the first year of our HBI grant project showed that serotonergic neurons are comprised of several molecular subtypes with distinct anatomical features, which suggests that they serve different functions in either a parallel or competitive manner. We will leverage on our findings to dissect the behavioral functions of distinct serotonergic neuron subtypes, using intersectional approaches for monitoring and manipulating the activity of specific serotonergic neuron subtypes combined with techniques for unbiased behavioral analysis. We will also investigate the organization of local circuits that mediate interactions between serotonergic subsystems. This work will provide further insights into the coordinated action of distinct cell types in the regulation of behaviors, and facilitate the discovery of improved strategies for treating bipolar disorder and other psychiatric illnesses.
 David Sinclair
David Sinclair
Professor of Genetics, Harvard Medical School
Copine 2, a novel risk gene for bipolar disorder
Bipolar disorder affects close to 6 million Americans. It is associated with accelerated aging and shorter life, yet the underlying biology remains unknown. We performed a genetic screen to identify human genes that control mitochondrial function. Out of 94 candidates, the CPNE2 gene, a protein of unknown function, was the most interesting. Importantly, genetic variants of CPNE2 gene are associated with an increased risk for BD and our mouse studies show that CPNE2 is primarily expressed in the brain. To study the physiological role of CPNE2, we generated knock-out mice. The mutants showed hyperactivity, impaired memory and anxiety—all of which are symptomatic of BD.
To verify the role of CPNE2 in the onset of BD, we will perform longitudinal behavioral studies of these mice to test for cyclicity of changes as well as validate the response to environmental stressors and pharmacological interventions. Armed with the latest molecular biology tools, we will pinpoint molecular mechanisms linking CPNE2 with behavioral impairment and BD. This study will provide deeper understanding about the biology and etiology of BD, and open new doors to therapeutic interventions.
 Jordan Smoller
Jordan Smoller
MGH Trustees Endowed Chair in Psychiatric Neuroscience; Professor of Psychiatry, Harvard Medical School; Professor of Epidemiology, T.H. Chan Harvard School of Public Health
Understanding the role of a novel genetic variant at the CACNA1C gene in bipolar disorder
Bipolar disorder is a complex disease that affects approximately 3% of the adult US population. Despite convincing evidence in support of genetic risk factors, causative mutations have yet to be discovered and therefore no conclusive genetic diagnostics are currently available.
Genetic studies, conducted in thousands of BD-affected individuals, have repeatedly implicated genes involved in calcium signaling, with some of the strongest and best replicated associations mapping to a calcium channel subunit encoding gene, CACNA1C. A novel genetic variant has been recently discovered in this gene. However, the role of this mutation has yet to be investigated in the context of BD, so the association with disease remains suggestive.
We hereby propose to apply pioneering methodology to more accurately characterize this particular CACNA1C mutation in DNA samples from BD patients and matched controls, and therefore investigate the relationship with disease status.
 Nao Uchida
Nao Uchida
Professor of Molecular and Cellular Biology, Harvard University
Competition between multiple dopamine systems as a model of bipolar disorders
Patients with bipolar disorder alternate between manic and depressive states. In manic states, patients exhibit hyper-exploration, novelty-seeking and increased motor activities. Dopamine-related drugs have been used to treat BD patients but the mechanism of action for these drugs has been difficult to understand, limiting rational design of treatment methods. Recent studies in animal models have indicated that there are multiple dopamine systems that serve distinct functions. Dopamine neurons projecting to the ventral striatum (VS) convey ‘canonical’ value signals, and promote reward-seeking behaviors. In contrast, DNs projecting to the posterior ‘tail’ of the striatum (TS) are activated by novelty and external threats, and promote avoidance behaviors.
In this project, we propose that exploratory behaviors including novelty-seeking are regulated by the balance between approach and avoidance behaviors promoted by distinct dopamine systems. More specifically, we hypothesize that TS dopamine promotes avoidance in response to novel stimuli whereas a different dopamine system promotes approach. In the last funding period, we have succeeded in verifying our hypothesis regarding TS. In this funding period, we will investigate the role of VS as well as other regions of the striatum in novelty exploration and a new foraging paradigm.
2018-2019 Awards
 Mark Andermann
Mark Andermann
Beth Israel Deaconess Medical Center
Modeling Mental Imagery in Bipolar Disorder:
Effects of dopamine on ongoing patterns of cortical activity
Recent pharmacological and genetic animal models of bipolar disorder suggest that increased levels of the neuromodulator dopamine may contribute to the hyperexcitability associated with mania. Human studies suggest that manic states also involve elevated levels of imagery of positive emotional experiences, while depressive states involve elevated imagery of negative emotional experiences. These symptoms are sometimes treated using drugs that block the actions of dopamine. However, the underlying neural circuit mechanisms remain unknown, in part because no animal models exist to study the neural circuitry underlying mental imagery.
We have recently refined methods to image neural activity in the same set of hundreds of individual cortical neurons in awake mice during and following engagement in a visual task involving rewards and mild punishments. Preliminary data gathered in the first year of our HBI grant project suggest that patterns of brain cells that are activated by positive or negative emotional visual experiences become re-activated in the subsequent periods of quiet waking in the dark, at higher rates than for reactivation of neutral visual experiences. We now plan to test whether reactivations of positive and negative experiences during quiet waking can be attenuated by manipulations of dopamine, and to dissect the specific brain circuits through which dopamine affects emotional mental imagery. This work will set the stage for precise therapeutic strategies targeted to specific cell types and circuits, thereby increasing efficacy and reducing side effects of future treatments for positive symptoms of bipolar disorder and other psychiatric diseases
 Todd Anthony
Todd Anthony
Boston Children’s Hospital
Connecting candidate bipolar disorder genetic risk factors to neural circuit-level phenotypes
Rare variations in the human genome are implicated in contributing to risk for developing Bipolar Disorder (BD). Ongoing sequencing efforts are identifying increasing numbers of such variations which track with affected status in families with multiple BD sufferers, but the rate at which such variants can be identified currently far exceeds that at which they can be tested to establish causality for particular symptoms, or to determine the neuronal cell types and circuits in which they act. As a step towards relieving this bottleneck, we will develop a novel rapid approach that enables candidate risk factor variants to be targeted to specific neuronal cell types in the mouse brain in order to define their function. Our focus will be on the lateral septum (LS), a region implicated in BD which rodent models have identified as a critical regulator of mood and motivation. We will test the hypothesis that a candidate BD mutation in a clinically relevant gene highly expressed in LS promotes persistent negative mood states and exerts opposite effects on the excitability of two distinct LS neuronal subsets that our previous Dauten-supported work revealed are differentially engaged by aversive stimuli.

 Joan A. Camprodon
Joan A. Camprodon
Mass General Hospital
Kerry J. Ressler
McLean Hospital
Structural plasticity underlying anhedonia in bipolar disorder treatment with electroconvulsive therapy
Electroconvulsive Therapy (ECT) is the most effective treatment in psychiatry, with response rates of 70-90% and indications for bipolar depression and mania. Despite its great efficacy and rapid action, the mechanisms underlying ECT remain unknown. Our programs study the effects of ECT in rodents and human patients separately, with a shared focus on reward circuitry which is critically affected in mania and depression.
Unipolar and bipolar depression is associated with different sets of symptoms. In particular, anhedonia, defined as the lack of enjoyment, reward, and pleasure, is important and difficult to treat. In patients treated with ECT, Dr. Camprodon’s lab has described volume increases in specific parts of the brain that underlie anhedonia. Separately, Dr. Ressler’s group has used a novel translational mouse model of ECT to identify an increase in the expression of synaptic plasticity molecules that mediate brain structural changes in these same brain regions.
Understanding the molecular and cellular mechanisms by which ECT improves the anhedonia symptoms in bipolar disorder is an important and potentially tractable problem in neuropsychiatry. This proposal will support a collaborative translational effort across our laboratories to study the effects of ECT on reward circuitry. Using the resolution available in our mouse model, we will study the structural and functional alterations in the brain in response to ECT. This study will be the first mechanistic examination of ECT-mediated recovery at the molecular, cellular and circuit level, with implications for future advances in understanding Bipolar Disorder and novel treatment approaches.
 Michael Tri H. Do
Michael Tri H. Do
Boston Children’s Hospital
A Circadian Control System for Counterbalancing Bipolar Disorder
Bipolar disorder and circadian rhythms are interlinked. Altered mood states can disrupt daily patterns of activity, but disruptions in these patterns also precede episodes of mania and depression. Moreover, artificial imposition of circadian structure can reduce symptoms of bipolar disorder—for example, regular periods of darkness can alleviate mania while light can mitigate depression. Indeed, light is the principal regulator of the circadian clock. The mechanisms by which light engages the clock are poorly understood. We are addressing this gap in knowledge by defining the pathway that connects the eye to the master clock in the brain. Our work will set the foundation for investigating whether this pathway is altered in bipolar disorder and how it may be leveraged to develop new treatments.
 Susan Dymecki
Susan Dymecki
Harvard Medical School
Understanding the role of serotonergic neurons in bipolar disorder circuitry
This project aims to delineate the specific serotonin (5HT)-producing subsystems in the brain that influence the opposing mania versus depression phases of bipolar disorder. Abnormalities in brain 5HT levels and the neurons that produce it are strongly linked to psychiatric illness, including bipolar disorder. We have recently found that the brain serotonergic system is comprised of functionally distinct subsystems, each specialized in the modulation of particular behavioral and physiological processes (e.g. anxiety-like behavior, aggression, sensorimotor gating, respiratory dynamics). In line with distinct functionalities, we also found distinguishing profiles of expressed genes. These findings reveal a subsystem responsive to neuropeptide Y (Npy) – a neurochemical also implicated in affective state. Through this seed grant, we will query the Npy2r-5HT subsystem in mouse models of depression-like traits versus mania-like traits elicited by chronic social defeat or positive winning experience, respectively. Genetic tools developed in the lab for cell-subtype-selective activity manipulation and cell marking will be used to probe the Npy2r-5HT subsystem at the organismal and circuit levels. Our preliminary findings—gathered in the first year of our HBI grant project—suggest that inhibition of Npy2r-5HT neurons safeguards against stress-associated dysfunctions, an outcome possibly akin to resilience. Paralleling anatomic studies, in which we visualize Npy2r-5HT neuron innervation targets, identify brain regions central to adult neurogenesis and arousal and stress responses, all of which are implicated in bipolar disorder. Here we test the functional link between Npy2r-5HT neuronal substrates and the behavioral outcomes mediated by this subsystem. Findings are expected to illuminate possibletherapeutically relevant substrates for protecting against depression- and mania-like symptoms.
 Bernardo Sabatini
Bernardo Sabatini
Harvard Medical School
Elucidating the role of distinct cell types of the dorsal raphe nucleus in bipolar disorder
The serotonergic system has been widely implicated in the pathogenesis of mood disorders, yet little is known about the mechanisms by which dysfunction of serotonergic neurons causes behavioral deficits. Although reduced serotonin signaling has been associated with bipolar disorder, there is a paradoxical involvement of serotonin in both depressive and manic behaviors.
The dorsal raphe nucleus houses the majority of serotonergic neurons in the brain. It is a heterogeneous structure comprised of many neuronal and non-neuronal cell types that interact with serotonergic neurons. Additionally, distinct subtypes of dorsal raphe serotonergic neurons may serve contrasting functions, potentially accounting for the serotonergic system’s role in seemingly opposing behavioral deficits. This heterogeneity adds complexity to the problem of understanding the function of the dorsal raphe nucleus in the etiology of bipolar disorder.
In this study, we will use high-throughput single cell RNA sequencing to capture changes in gene expression across multiple cell types in the dorsal raphe nucleus. We will assess the transcriptional changes induced by stress and other perturbations that model both depressive and manic behaviors. We will also investigate the role of specific serotonergic neuron subtypes in the regulation of impulsivity and hyperactivity, two major features of manic behavior, by using intersectional viral and genetic tools to record the activity of these specific populations. This work will allow us to better understand the simultaneous involvement of multiple dorsal raphe cell types in the regulation of behaviors and the pathophysiology of bipolar disorder.
 Beth Stevens
Beth Stevens
Boston Children’s Hospital
High-content, super-resolution synapse analysis in human prefrontal cortex
Synaptic pruning, a normal process by which extra synapses are eliminated, occurs throughout the mammalian brain during fetal and early postnatal development, but in the human prefrontal cortex is most pronounced during adolescence. A longstanding hypothesis is that aberrant synaptic pruning in the adolescent cortex may contribute to the onset of bipolar disorder and schizophrenia during this developmental period. Several studies have found small but significant reductions in synapse numbers in the brains of patients compared to healthy controls, consistent with over-pruning. However, these studies have been limited by the small number of available postmortem patient brain samples, especially for bipolar disorder, as well as by the low-throughput nature of age-old methods for counting synapses. To address these critical limitations, we are collaborating with colleagues at the Stanley Center for Psychiatric Research at the Broad Institute of MIT and Harvard to develop new techniques for synapse counting and analysis, which we will apply to a large cohort of patient and control brain tissue samples from the Stanley Medical Research Institute. Specifically, we are working with the MIT labs of Ed Boyden and Mark Bathe to modify tissue expansion and barcoded antibody methods for combined application in human tissue, which will enable high-content, super-resolution synapse analyses: by imaging a large number of synaptic proteins simultaneously, we will be able to take an unbiased “census” of many synapse types in patient and healthy control brains, while also investigating cellular mechanisms of aberrant pruning.
 Naoshige Uchida
Naoshige Uchida
Faculty of Arts and Sciences, Harvard University
Competition between multiple dopamine systems as a model of bipolar disorders
Patients of bipolar disorder (BD) alternate between manic and depressive states. In manic states, patients tend to seek new and exciting stimulation, called novelty seeking and hyper-exploration. It has been thought that dopamine is released during these situations, and the drugs that affect dopamine transmissions in the brain are known to ameliorate symptoms of bipolar disorders. However, the actions of these drugs have been difficult to understand and largely anecdotal, preventing rational treatment methods.
Much of the work on dopamine has been guided by the dogma that dopamine neurons encode reward prediction errors (RPE = actual minus expected reward) and that they do so in a uniform manner. However, work from several groups, including ours, now indicates that dopamine neurons projecting to different targets exhibit distinct properties and serve distinct functions. These new data on the multiple dopamine system raises the possibility that this new knowledge can greatly improve our understanding of the neural mechanisms underlying BD. Here, we propose that exploratory behaviors including novelty-seeking are regulated by the balance between approach and avoidance behaviors promoted by the two distinct dopamine systems (dopamine in the ventral striatum [VS] versus the tail of the striatum [TS]). We hypothesize that VS dopamine promotes approach whereas TD dopamine promotes ‘timidity’ and avoidance in response to novel stimuli. Our results, if true, will raise the possibility that alternations between manic and depressive states in BD are caused by unbalance between the VS and TS dopamine, and provide a foundation toward mechanistic understanding of BD.
 Charles J. Weitz
Charles J. Weitz
Harvard Medical School
Cytoplasmic circadian clock complexes in mammals:
Could they be autonomous post-translational oscillators?
Circadian clocks are internal oscillators that drive daily biological rhythms. Such clocks are found in animals, plants, fungi, and bacteria called cyanobacteria. In mammals, circadian clocks are found in the brain and in all peripheral tissues. These distributed clocks govern the daily timing of our physiology and behavior, and it has long been known that abnormal circadian rhythms are associated with mood disorders. Recent human genetic and anti-depressive drug studies have further suggested that abnormal circadian clocks might contribute causally to bipolar disorder. The nature of the abnormality is unknown.
Circadian clocks of animals, plants, and fungi are built on a transcriptional feedback loop, a process in cells in which the handful of circadian clock proteins periodically inhibit their own production, generating 24-hour molecular rhythms. Cyanobacteria have a circadian feedback loop, but it turns out to be of minor importance. Cyanobacterial clock proteins, in addition to participating in the feedback loop, also work together to generate a molecular rhythm purely at the protein level (“post-translational”), now known to be the predominant factor for cyanobacterial rhythms.
Might mammalian clock proteins have a similar but unknown action? This project proposes to test the hypothesis that an intrinsic post-translational oscillator is present within the mammalian circadian clock. It takes advantage of biochemical tools we have developed to study the mammalian circadian clock, and insights we gained during our earlier HBI bipolar grant project. If the hypothesis is correct, the result will fundamentally change our conception of the circadian clock and open new avenues to explore the connection between circadian clock dysfunction and bipolar disorder.
 Tracy Young-Pearse
Tracy Young-Pearse
Brigham and Women’s Hospital
Targeting Bipolar Disorder Genes in Human Neurons in a Dish
Bipolar disorder is characterized by severe and unusual shifts in mood, energy and activity levels. Both genetic and environmental factors play a role in the onset of disease, but the cell and molecular mechanisms underlying the disease are poorly understood. Genetic studies provide the field with valuable clues to the causes of bipolar disorder. Under this award, we will use a new technology to genetically engineer human stem cells to introduce mutations in specific genes that cause bipolar disorder. We then will take these stem cells and use them to make human brain cells in a dish. We will compare brain cells with the mutations to those without the mutation, to examine how these mutations affect brain cell development. By understanding how bipolar brain cells are different, we hope to identify new therapeutic strategies for this disorder.
2017-2018 Awards
 Mark Andermann
Mark Andermann
Beth Israel Deaconess Medical Center
Modeling mental imagery in bipolar disorder
Recent pharmacological and genetic animal models of bipolar disorder suggest that increased levels of the neuromodulator dopamine may contribute to the hyperexcitability associated with mania. Human studies suggest that manic states also involve elevated levels of imagery of positive emotional experiences, while depressive states elevated imagery of negative emotional experiences. These symptoms can be treated with drugs that block the actions of dopamine. The underlying neural circuit mechanisms remain unknown, in part because no animal models exist to study the neural circuitry underlying mental imagery. We have developed methods to track the activity of the same set of hundreds of individual brain cells in awake mice across weeks. In this proposal, we will test whether patterns of brain cells that are activated by positive or negative emotional experiences become re-activated in the quiet periods following these experiences. We will then test whether this surrogate of emotional imagery can be attenuated by blockade of dopamine. If so, we will then attempt to pinpoint the precise brain circuits through which dopamine affects emotional mental imagery. This work will set the stage for precise therapeutic strategies targeted to specific neurons and circuits, thereby increasing efficacy and reducing side effects.

 Justin Baker and Dost Öngür
Justin Baker and Dost Öngür
McLean Hospital
Circuit dynamics underlying longitudinal fluctuations in mood and cognition in bipolar patients
Even at “baseline” individuals with bipolar disorder often show fluctuations in mood and cognition that may be picked up by others (e.g., an astute caregiver or family member), and may represent the early warning signs of an impending episode of mania or depression. Until recently, technical and logistical challenges have prevented the careful study of these fluctuations and the factors that drive them. Over the past year, we have developed a robust “deep phenotyping” platform to track symptoms, behavior and neurobiology of individuals over extended periods by combining continuous data from smartphones and wearable devices with repeated neuroimaging and conventional study visits. We have already learned how to deploy this powerful approach in individuals with clinically significant bipolar illness, yielding important insights about the stability of our measurements and about the relationships between neurobiological change and behavioral change. In the present study, we will build and test individual-specific models that combine neurobiological, behavioral, and environmental factors to explain and even predict changes in mood and cognition. This project is intended as the precursor for real-time, individually tailored illness detection systems that could pick up on early warning signs and deliver warnings to the patient, a family member, and/or a preferred care giver to avoid costly clinical outcomes and engage the individual in their own recovery.
 Michael Crickmore
Michael Crickmore
Boston Children’s Hospital
Linking the mitochondrial dysfunction and dopamine hypotheses of bipolar disorder
Two prominent hypotheses about the root cause of bipolar disorder are the mitochondrial dysfunction hypothesis and the dopamine hypothesis. My lab is exploring a potential unification of these two hypotheses. Bipolar patients show many signs of mitochondrial dysfunction in the brain, one of which is an increase in lactate production. High lactate levels likely reflect an increase in glycolysis, which indicates that oxidative phosphorylation in mitochondria is not able to produce enough ATP to meet the energy demands of the neurons. Aside from its role in storing chemical energy, ATP is also used as a signaling molecule. For example, intracellular ATP closes KATP potassium channels. Several studies in nonneuronal tissues have shown that pyruvate kinase (Pyk, the terminal kinase in glycolysis that phosphorylates ADP to make ATP), is present in KATP complexes. In an unbiased screen for genes that regulated a dopamine-mediated motivated behavior, we unexpectedly hit Pyk. We then found that the two core subunits of KATP channels also regulate motivation in this system. Our working hypothesis is that localized glycolysis in the vicinity of KATP channels sculpts the output of dopaminergic activity so that it is appropriate for the internal state of the animal. The shift to glycolysis seen in bipolar disorder may result in altered activity of KATP channels, which I propose regulate dopaminergic circuitries that control our moods and behaviors.
 Susan Dymecki
Susan Dymecki
Harvard Medical School
Understanding the role of serotonergic neurons in bipolar disorder circuitry
The goal of this project is to delineate the specific serotonin-producing subsystems in the brain that influence the opposing mania versus depression phases of bipolar disorder. Abnormalities in brain serotonin levels and the neurons that produce it have been strongly linked to psychiatric illness, including bipolar disorder. We have recently found in rodent models that the brain serotonergic neuronal system is comprised of functionally distinct subsystems, each specialized in the modulation of particular behavioral and physiological processes (e.g. anxiety-like behavior, aggression, sensorimotor gating, respiratory dynamics). In line with distinct functionalities, we also found distinguishing profiles of expressed genes. In certain cases, these findings have pointed to subsystem responsiveness to other neuromodulators such as dopamine or neuropeptide Y – neurochemicals also implicated in affective state. Through this seed grant, we will query two serotonergic subsystems – the Drd2/5-HT subsystem and the Npy2R/5-HT subsystem – in recently developed models of depression-like traits versus mania-like traits elicited by chronic social defeat experience or chronic positive winning, respectively. Innovative genetic tools developed in the lab for subsystem activity manipulation and cell marking will be used to probe subsystem function at the organismal and circuit levels. A deeper understanding of these neuronal subsystems and their interplay with other neuromodulators may lead to new substrates for protecting against depression- and mania-like symptoms.
 Corey Harwell
Corey Harwell
Harvard Medical School
Understanding Hippocampal Neurogenesis for the Treatment of Psychiatric Disease
Hippocampal circuit function has been shown to be important for a variety of cognitive and behavioral functions including learning and memory. The hippocampus is also unique in that it contains a population of neuronal progenitor cells capable of producing new granule neurons throughout adulthood. These newly generated neurons integrate into the existing circuits of the hippocampus where they are required for hippocampal circuit function. Reduced adult hippocampal neurogenesis is implicated in the pathogenesis of variety of psychiatric diseases in humans including major depression and bipolar disorder. However the circuit mechanisms and signaling pathways that regulate adult neurogenesis is still not understood. It has long been known that secreted growth factor signaling can promote hippocampal neurogenesis, but their mechanism of action remains unknown. We have identified a subset of growth factor expressing neurons that project into the hippocampus where they may function to regulate hippocampal circuit activity and neurogenesis. We plan to test whether neuronal activity and growth factor release from this subset of neurons is necessary and sufficient to promote hippocampal neurogenesis and resistance to depression related behaviors. The results from these studies will provide a deeper understanding of the molecular pathways and brain circuits that regulate adult neurogenesis and provide new targets for therapeutic treatments of psychiatric disease.
 Pascal Kaeser
Pascal Kaeser
Harvard Medical School
Structural roles of calcium channels in the brain and their disruption in bipolar disorder
Bipolar disorder is a severe brain disorder that affects about 3% of the American population, but its causes and pathophysiology are not well understood. In recent years, human genetic studies have found that mutations in brain calcium channels are strongly associated with bipolar disorder. A well understood function of calcium channels in the brain is their role in mediating activity induced calcium influx into nerve cells. However recent data suggest that calcium channels may have additional structural roles for nerve cells by building protein complexes that are important for brain wiring and signaling. A leading hypothesis is that these structural roles are mediated through interactions with scaffolding proteins, but these roles are not well understood. Compellingly, some of the scaffolding proteins that we have found to interact with brain calcium channels are also associated with bipolar disorder in human genetic studies. Thus, we hypothesize that calcium channels operate in a structural scaffolding network, and that disruption of this network contributes to the pathogenesis of bipolar disorder. We use a broad spectrum of methods including brain biochemistry, mouse gene targeting, electrophysiology and imaging to dissect the roles of calcium channels and interacting proteins in scaffolding. Our work will reveal new mechanisms of calcium channel function and will likely provide insight into how calcium channels and interacting proteins contribute to the pathophysiology of bipolar disorder.
 Bence Olveczky
Bence Olveczky
Harvard Faculty of Arts and Sciences
Analyzing the relationship between neural activity and behavior in rodent models of bipolar disorder
Bipolar disorder and other mental illnesses are caused by deficits in neural circuit function. Our ability to treat the underlying pathologies is contingent on better understanding how neural circuits fail in different disorders, and how these failure modes lead to altered behavior. Rodent models of psychiatric disease hold promise in this regard, but capitalizing on it will require measuring neural activity and behavior simultaneously and at high resolution over timescales relevant for mood disorders (i.e. days and weeks), something not feasible with current technology. To enable this, we will develop an innovative experimental platform for recording activity from many neurons in different parts of the brain continuously over weeks and months in freely behaving animals. High-resolution behavioral data from accelerometers and a video-based motion capture system will be collected simultaneously. Our system will be completely automated, including unsupervised extraction of behavioral and neural states, thus allowing for efficient and high-throughput experimental approaches and unbiased analysis of resulting data. We will use our system to relate changes in brain activity to changes in behavior, and observe the effects of various disease states and mood-stabilizing drugs, thus making important progress towards a neural circuit-level understanding of psychiatric disorders.
 Tracey Petryshen
Tracey Petryshen
Massachusetts General Hospital
Human iPSC Models to Bridge Gene Discovery and Neurobiological Mechanisms in Bipolar Disorder
Recent human genetic studies have been remarkably successful in identifying sequence changes in the genome that increase the risk of developing bipolar disorder. However, it is unknown how these genetic variants contribute to the disease. This project will leverage recent landmark studies and technological innovations to develop a biological platform to investigate the effects of these genetic variants in human neurons. The ankyrin 3 gene (ANK3), one of the strongest bipolar disorder risk genes, will serve as a prototype to develop this platform. The latest information regarding functional elements in the genome will be used to identify genetic variants in ANK3 that are likely to be deleterious. Using advanced genome editing technology, human induced pluripotent stem cells (iPSCs) will be engineered to carry the selected ANK3 genetic variants. Following differentiation of the iPSCs into functioning neurons, molecular and cellular functions will be studied to delineate how the ANK3 genetic variants on may contribute to disease. This project is expected to bridge a gap between the genetics and neurobiology of bipolar disorder by delivering a biological platform for studying genetic risk variants in human neurons.
 Uwe Rudolph and Vadim Y. Bolshakov
Uwe Rudolph and Vadim Y. Bolshakov
McLean Hospital
From genetic variant to disease biology: elucidating a genomic rearrangement associated with bipolar disorder
In a large study looking for variations in the copy number of genes in patients with bipolar disorder, others have identified additional copies of 15 genes in a defined chromosomal region, 9p24.1, including 4 (instead of the normal 2) copies of the GLDC gene encoding glycine decarboxylase, an enzyme which degrades glycine. Glycine is a co-agonist at excitatory NMDA receptors in the brain. Our hypothesis is that the extra copies of GLDC increase degradation of glycine, and thus result in hypofunction of NMDA receptors and of NMDA receptor-dependent synaptic plasticity. We have generated mice which mimic the genetic copy number changes seen in patients. These mice display behavioral changes consistent with neurodevelopmental dysfunctions. In the brain, GLDC is only expressed in astrocytes. We therefore want to test the hypothesis that there is a local glycine deficit in astrocytes and that glycine release from activated astrocytes is reduced, which then results in hypofunction of NMDA receptors on nerve cells. In addition, we are analyzing changes in global gene expression patterns. Using bioinformatics analysis, we will evaluate whether biochemical risk pathways for neurodevelopmental disorders or other biological parameters are affected by the mutation. Finally, we plan to generate a mouse line in which the increase in copy number is restricted to the GLDC gene. This novel mouse line will enable us to unequivocally determine whether all or only part of the phenotypic changes observed are due to the extra copies of GLDC and not the extra copies of other genes in this chromosomal region. In summary, we plan to provide a direct link from a genetic variant to biochemical pathways, to synaptic functions, and to disease biology.
 Hisashi Umemori
Hisashi Umemori
Boston Children’s Hospital
Protocadherin-17 Dysregulation and Bipolar Disorder
Protocadherin-17 (Pcdh17) is a cell-cell adhesion molecule that is highly expressed in the developing brain. Single nucleotide polymorphisms (SNPs), a type of genetic variation among people, in the Pcdh17 gene are significantly correlated with human bipolar disorder. These SNPs may cause dysregulation of Pcdh17 expression. However, whether dysregulation of Pcdh17 expression affects brain development and contributes to bipolar disorder remains to be elucidated. We hypothesize that dysregulated Pcdh17 expression impairs neuron-neuron connections that underlie the regulation of mood, leading to bipolar disorder. We will test our hypothesis by creating novel animal models in which Pcdh17 expression is dysregulated and performing in vitro and in vivo experiments.
2015-2016 Awards
 Todd Anthony
Todd AnthonyBoston Children’s Hospital
Imaging activity in a neural circuit that controls behavioral indices of anxiety and bipolar disorder
Bipolar disorder is characterized by alternating bouts of depression and mania, and commonly co-occurs together with anxiety disorders. Although the neural circuit-level mechanisms that underlie these illnesses are unknown, abnormal activity in related, possibly overlapping neuronal subpopulations may be responsible. We have identified a neural circuit in the lateral septum (LS), a brain region implicated in human bipolar disorder whose activity can promote both anxiety and depression in mouse behavioral tests. To determine how neurons in this circuit are capable of mediating these distinct behaviors, we will optically record their activity with cellular resolution while mice are undergoing behavioral tests that measure indices of anxiety and depression. We anticipate that these imaging experiments will yield valuable information that will lay the foundation for future studies of LS control of mood states, and the ways in which abnormal activity in this circuit may influence susceptibility to psychiatric disorders.
 Paola Arlotta
Paola Arlotta
Harvard Faculty of Arts and Sciences
Understanding the neuronal substrate of bipolar disorder
Many sites in the human genome associated with an increased risk of bipolar disorder have been identified, and additional sequencing efforts are ongoing. There is a strong need for strategies to mine this wealth of genetic information to understand disease etiology and progression, as well as to inform treatment strategies. One major obstacle is that the particular neurons and circuits affected in bipolar disorder are not known—nor is it known whether the disease has a developmental origin. Our goal is to determine whether regions of the genome mutated in people with bipolar disorder are enriched for genes specifically expressed in distinct neuronal populations. We propose to build a database cataloging which genes are turned on and off in different neuronal classes at different developmental stages. Neurons will be isolated from both the mouse cortex and from human cerebral organoids derived from pluripotent stem cells. These cerebral organoids, although cultured in a dish, recapitulate some aspects of normal brain development. We expect that as the number of profiled neuronal classes grows, this type of resource will provide a platform to help identify which types of neurons are affected and when in development bipolar disorder is initiated.
 Chinfei Chen
Chinfei Chen
Boston Children’s Hospital
Circuit-based approach to understanding bipolar disorder
One characteristic symptom of bipolar disorder is dramatic and abnormal mood swings. This feature often becomes evident during adolescence. We aim to test the hypothesis that aberrant wiring between neurons in the cortex and subcortical regions of the brain can contribute to such difficulty in modulating mood. Connections between the cortex and the amygdala, a deep brain region important for emotions, are relayed through a subcortical hub called the thalamus. The thalamus serves as a gatekeeper or switchboard operator for information flow and therefore can modulate emotion. Neuronal connections between cortex and thalamus are known to develop during the adolescent years in humans and in mice. Here we will characterize the basic formation and maturation of this connection in mice using electrophysiological recordings in brain slices. We will also test whether transient disturbance of the cortex in adolescent mice can alter the wiring between cortex, thalamus, and amygdala. The results from these studies will help establish how brain circuits gating emotions develop normally and abnormally.
 Michael Crickmore
Michael Crickmore
Boston Children’s Hospital
Gaining control of dopamine levels to combat bipolar disorder
Aberrantly high and low dopamine levels are implicated in the manic and depressive phases of bipolar disorder, respectively. Many of the treatments for psychological disorders—including bipolar disorder—target dopaminergic signaling, demonstrating the efficacy of intervening in this system. We have developed a novel system with a sensitive behavioral readout of dopamine levels in the fruit fly, where powerful genetic tools are available. We are undertaking a molecular and circuit-level interrogation of this system as a means of discovering new principles of dopaminergic control that will be relevant to understanding and treating the motivational swings associated with bipolar disorder.
 Pascal Kaeser
Pascal Kaeser
Harvard Medical School
Structural roles of calcium channels in assembling synapses and their disruption in bipolar disorder
In recent years, human genetic studies have found that mutations in calcium channels in the brain are strongly associated with bipolar disorder. Our recent data, together with studies from other laboratories, suggest that calcium channels may play structural roles in nerve cells by building protein complexes that are important for brain wiring and signaling. Compellingly, some of the proteins that we have found to interact with brain calcium channels are also associated with bipolar disorder. We hypothesize that calcium channels operate in a structural scaffolding network, and that disruption of this network contributes to the pathogenesis of bipolar disorder. We use a broad spectrum of methods including brain biochemistry, mouse gene targeting, electrophysiology, and imaging to dissect the roles of calcium channels and interacting proteins in scaffolding. Our work will reveal new mechanisms of calcium channel function and will likely provide insight into how calcium channels contribute to the pathophysiology of bipolar disorder.
 Margaret Livingstone
Margaret Livingstone
Harvard Medical School
Focused ultrasound for treatment of psychiatric diseases
Psychiatrists lack non-invasive, safe, highly-specific, and reversible techniques to modulate brain activity in mood disorders and other diseases. We have developed a novel technique that accomplishes this in rats. The goal of this proposal is to extend this neuromodulation technique to a primate. The technique is to use focused ultrasound to permeabilize the blood- brain barrier (BBB) at a target site in the brain, and then to systemically administer a neuromodulatory substance that is active in the brain, ineffective in the periphery, and does not normally cross the BBB. Neuromodulation will therefore occur only at the sonicated site and nowhere else. Whereas neurosurgeons are currently exploring the potential for treating many neuropsychiatric disorders with deep brain stimulation, our approach can be safely tested for efficacy in psychiatric diseases without brain surgery.
 Alexander Schier
Alexander Schier
Harvard Faculty of Arts and Science
Functional analysis of genes associated with bipolar disorder
The functions of the genes that have been implicated in causing bipolar disorder are largely unknown. Zebrafish are a powerful model system to determine the function of genes because gene activity can be easily manipulated and resulting changes in behavior, anatomy, and brain activity can be analyzed very efficiently. This project will mutate in zebrafish twenty genes associated with bipolar disorder and determine their functions, as well as assess how eight common drugs used to treat bipolar disorder affect the brain and behavior.
 Hisashi Umemori
Hisashi Umemori
Boston Children’s Hospital
Excitatory and inhibitory synaptic organizers and bipolar disorder
In order for the brain to function properly, neurons must establish a balanced network of excitatory and inhibitory synapses. We have recently identified two related molecules (called Fibroblast Growth Factors, FGF22 and FGF7) that promote excitatory versus inhibitory synapse formation in the mammalian brain. We further found that mice lacking one of these molecules (FGF22) exhibit depression-like behavior, while mice deficient in the other (FGF7) show manic-like behavior. Other lines of evidence also link the signaling of FGF molecules to bipolar disorder. Here our goal is to determine how these FGFs contribute to neural circuit formation and mood disorders. Our work will reveal the molecular mechanisms underlying balanced synaptic network formation in the mammalian brain and suggest novel strategies for treating bipolar disorder.
 Charles Weitz
Charles Weitz
Harvard Medical School
Is an autonomous protein oscillator embedded in the mammalian circadian clock?
The goal of the project is to provide new insights into the circadian clock, the body’s daily timekeeping system. The circadian clock is responsible for our myriad daily rhythms, the most obvious of which is the sleep-wake cycle. Abnormalities of the circadian clock have been strongly linked to bipolar disorder and other mood disorders, but the nature of the relationship between the clock and mood regulation is obscure. Deeper understanding of the circadian clock could ultimately reveal the nature of this link, leading to completely new approaches to the diagnosis and treatment of bipolar disorder.
 Alik Widge
Alik Widge
Massachusetts General Hospital
Engineering brain rhythms to improve emotion regulation
A core feature of bipolar disorders is a disruption of emotion regulation. Both the depressed and the (hypo)manic phase involve difficulties regulating one’s emotional responses to everyday situations. Brain imaging work has linked this to a failure of prefrontal cortex to control neuronal firing in the amygdala, as measured by poor connectivity between these structures. The disrupted connectivity is still present even when patients are “well” on medications, suggesting that it may be one of the neurologic causes of bipolar disorder. It might also explain why patients who are at the “right” mood level still show problems with impulsivity and mild mood swings. Our laboratory is developing electrical brain stimulation technologies that we think may be able to reduce or reverse this prefrontal cortex-amygdala circuit deficit. In stroke and spinal cord rehabilitation, other investigators have found that brain regions can be “re-wired” together by recording in one and stimulating in the other with very precise timing. Our group, which blends engineers and neuroscientists, will develop software and hardware tools to do combined recording and stimulating (“closed loop”) re-wiring between prefrontal cortex and amygdala. This first year of experiments will use a rat model, with a fear-conditioning test that is known to be sensitive to this specific connection. If this succeeds, the PI is a psychiatrist who works with a variety of deep brain stimulation technologies, and we will be able to work quickly towards human translation.
Banner image shows serotonergic neurons in dorsal raphe nucleus of a mouse brain, courtesy of Olga Alekseyenko in the lab of Susan Dymecki