ALS Grants
The Harvard Brain Science Initiative is grateful for the generous support of the Stephen Van R. Winthrop Fund for ALS Research, which has funded four cycles of seed grants for the HBI community to date. These grants have supported the launch of 20 different seed projects, funding 22 outstanding investigators across the university with diverse areas of expertise in neuroscience—ranging from cellular and molecular biology, physiology, microbiology and immunobiology to genetics, stem cell biology and translational medicine. You can read more about each project below.
2021-2022 Awards
 Jun Huh
Jun Huh
Determining the contribution of gut microbiota in amyotrophic lateral sclerosis
Recent data from preclinical studies with mouse models of amyotrophic lateral sclerosis (ALS) suggest a connection between mouse gut bacteria and the development of neurodegenerative phenotypes; however, the role of gut bacteria in ALS patients is not well understood. The human intestine contains a myriad of bacteria that influence various aspects of human physiology, from immune responses to brain function. Thus, we hypothesize that specific types of gut bacteria derived from human ALS patients contribute to ALS phenotypes. To test our hypothesis, we aim to identify gut bacteria from human ALS patients, which are positively or negatively correlated with ALS progression. We will then introduce these human-derived bacteria into ALS mouse models, rederived into a germ-free condition, and investigate if they exacerbate or mitigate ALS-like symptoms. Our proposed research has the potential to uncover the underlying mechanisms by which specific microbes contribute to the development of neurodegenerative phenotypes and give rise to new strategies for diagnosing and treating ALS.
 Maria K. Lehtinen
Maria K. Lehtinen
Examining the choroid plexus in ALS—a novel site of pathology
Amyotrophic lateral sclerosis (ALS) is a progressive, incurable, and ultimately fatal neurologic disease. Alongside classic symptoms of progressive paralysis and muscle atrophy, patients show signs of aberrant neural inflammation. Current treatments, including riluzole, a sodium channel blocker given in combination with vitamins, target symptoms but do not slow progression or significantly prolong life. The cause of ALS in many cases is unclear; however, hexanucleotide expansion in C9orf72 is commonly found in familial ALS. Moreover, ALS disease features are recapitulated in C9orf72-deficient mice. Recent findings show that reducing systemic and neural inflammation in C9orf72-deficient mice can prevent premature mortality. These findings suggest the possibility of developing treatments to target disease progression. A detailed understanding of the source of inflammation could reveal new therapeutic targets to interrupt these processes. A promising starting point for this work comes from recent observations of choroid plexus (ChP) tissue from ALS patients, showing perturbations of ChP structure and function as a novel aspect of ALS pathology. Using C9orf72 mice, we will elucidate the ChP inflammatory response by histological and in vivo imaging approaches. This proposal will open a new avenue in ALS research, and provide a foundation for testing pharmacological tools for mitigating neuroinflammation in ALS.
 Robin Reed
Robin Reed
Identification of a cellular pathway disrupted by multiple ALS-causative genes
Mutations in numerous genes cause ALS, and these genes function in many different cellular pathways. We recently discovered that a common cellular pathway is disrupted across multiple forms of ALS. This pathway, which plays an essential role in immune regulation, is disrupted by RNA-binding protein mutations known to cause ALS, as well as expansion mutations of the C9ORF72 gene—which are responsible for the largest proportion of heritable ALS. Our overarching goal for this seed project is to understand this pathway better, so that we might gain insights into the development of broadly-applicable therapeutics.
 Rosalind Segal
Rosalind Segal
The RNA-binding protein SFPQ in ALS
ALS can run in families, but most ALS patients do not have a family history of the disease. However, mutations found in families with ALS provide clues into the abnormalities that cause loss of motor neurons and lead to an inability to move. Several ALS families have mutations in proteins that attach to RNA molecules. We found that one of these ALS-associated proteins acts both in the cell nucleus and in the long axons of motor neurons. Axons connect motor neurons to other nerve cells, and connect motor neurons to muscles; the ALS-associated protein helps RNAs move through these long axons. We will identify the RNAs that this ALS-associated protein attaches to, and we will see if this protein must be active in the axon in order to keep motor neurons alive and healthy. Together the studies proposed will help us understand how changes in RNA movement within motor neurons can cause ALS, and give us new ideas on ways to treat this devastating disease.
 Pamela Silver
Pamela Silver
Engineered hormone to suppress neuron degeneration in ALS
ALS is a neurodegenerative disease affecting neurons in the brain and spinal cord. In vitro and in vivo models of ALS have shown that the protein erythropoietin is neuroprotective. Erythropoietin has been explored as an ALS treatment in animals and human clinical trials. Two problems have limited its use. It stimulates blood clotting even at low doses, while its neuroprotection occurs at high doses. Thus, doses needed for ALS treatment are considered unsafe. Our aim is to develop an engineered protein with the neuroprotective activity of erythropoietin, but without the blood-clotting side effects. Our molecule will have a long lifetime in the body so that it does not require frequent dosing and will be compatible with practical use by patients. We will base our molecules on the three-dimensional structures and models of erythropoietin and its receptors and include other engineered protein features to enhance safety and convenience. During the funded period, we will test our proteins for the ability to promote survival of cultured neuronal cells and for protective activity in a genetically engineered mouse that suffers from ALS. The overall goal is to provide a protein engineering solution to address the needs of ALS patients.
2017-2018 Awards
 The role of microbiota in ALS pathology
The role of microbiota in ALS pathology
Isaac Chiu, Assistant Professor of Microbiology & Immunobiology, Harvard Medical School
Mammalian hosts intimately interface with trillions of gut-resident commensal bacteria. It is increasingly clear that molecular interactions between the gut microbiota and the nervous system play a key role in regulating neural function and CNS inflammation through a gut-brain axis. Recent work has shown that the components of the microbiota can drive neurodegeneration in mouse models of Parkinson’s and Alzheimer’s disease. We hypothesize that dysregulation of the microbiota occurs in ALS, leading to increased neuro-inflammation, microglia activation and accelerated motor neuron degeneration. In this project, we aim to investigate whether gut microbial communities are dysregulated in mouse models of ALS. We will determine whether targeted modulation of the microbiome alters spinal cord inflammation, neuronal loss, and disease progression in ALS transgenic mice. We have extensive experience analyzing immune responses and the role of microglia in ALS, and our laboratory is deeply interested on the role of microbe-neuron interactions in inflammation and disease. This new project allows us to study how the microbiota play a role in neurodegeneration in ALS—which could open up new avenues to treat this devastating disease, perhaps via the targeting of specific microbes or their mediators to modulate inflammation and neurotoxicity.

 Permanent inactivation of the C9orf72 ALS mutation in cells from human patients
Permanent inactivation of the C9orf72 ALS mutation in cells from human patients
James Gusella, Bullard Professor of Neurogenetics, Harvard Medical School and Massachusetts General Hospital
Jong-Min Lee, Assistant Professor of Neurology, Harvard Medical School and Massachusetts General Hospital
Knowledge of the genetic cause of a late-onset disease opens the potential for developing effective treatments. However, the traditional route of defining the biological mechanisms by which the mutation leads to disease symptoms and then addressing these with small molecule drugs has proved a very long, complex and uncertain path. In dominant genetic disorders, a single copy of the mutation is sufficient to cause the disease even though the second copy of the gene is completely normal. Therefore, an ideal treatment to eliminate all consequences of the disease mutation might be to permanently inactivate the mutant gene while leaving the normal version of the gene untouched. Using stem cells from subjects with the ALS-causing mutation in a gene called C9orf72, we will use CRISPR, a powerful technique for editing the sequence of the genome, to prevent only the expression of the mutant version of the gene. Our proof-of-principle experiments will provide a first step toward development of this therapeutic strategy while also producing paired lines of mutant and normal stem cells for investigating the effects of C9orf72 mutation in an accurate, human-derived model system.
 Single molecule approaches to understanding protein aggregation in ALS
Single molecule approaches to understanding protein aggregation in ALS
Ying Lu, Assistant Professor of Systems Biology, Harvard Medical School
ALS is a neurodegenerative disorder characterized by pathological protein aggregation in motor neurons. In healthy circumstances, the ubiquitin-proteasome system (UPS) scavenges abnormal or unwanted proteins and removes them from cells. A failure in this clearance system can cause protein accumulation and aggregation, which may eventually lead to ALS. Efforts to ameliorate ALS have focused on eliminating large aggregates that are readily detectable under a microscope. So far, the success of such measures has been very limited—suggesting that we need a better understanding of the protein aggregation process and associated toxicity. We are taking a two-pronged approach to this problem. First, we wish to elucidate the mechanisms behind pathological protein aggregation in ALS. Because we recognize that the process of aggregation involves multiple steps that occur sequentially, we are using single-molecule fluorescence approaches, along with mathematical modeling, to examine individual steps and factors in this process. Several key questions in the field may benefit from our analysis: For instance, what underlies the transition from reversible to irreversible protein aggregation? How may an aggregated protein become an inhibitor of the UPS? Why does the tendency of proteins to aggregate vary dramatically across tissues? Second, we wish to examine the growing evidence that smaller, harder to visualize protein aggregates may be highly toxic in ALS. Building on our past studies, we will investigate how the UPS degrades these small aggregates—and how a failure to do so may result in inhibition of the UPS and a rapid accumulation of pathological protein aggregates.
 Investigating hspA4L in ALS patient motor neurons – a novel therapeutic target for a common pathological problem
Investigating hspA4L in ALS patient motor neurons – a novel therapeutic target for a common pathological problem
Lee Rubin, Professor of Stem Cell and Regenerative Biology and HSCI Director of Translational Medicine, Harvard University
A prominent pathological feature of both familial and sporadic ALS is the accumulation within spinal cord motor neurons of aggregated, misfolded proteins. It is generally believed that therapeutics that reduce aggregation could be beneficial for diseased motor neurons. In fact, cells have evolved pathways for preventing aggregation, but they appear to malfunction in ALS. One particular protein, known as HSP4AL, has been shown to act as an anti-aggregation factor, and experiments in fly and mouse models of ALS suggest that increasing its levels may improve neuronal survival. However, it is very important to determine if this is also true in human neurons. Thus, we will study the function of this protein in motor neurons produced from ALS patient iPSCs (induced pluripotent stem cells). Our experiments will establish whether high levels of HSP4AL can also stop proteins from aggregating in motor neurons and, by doing so, prevent them from dying. These studies could provide support for the notion that HSP4AL is a valid target for the treatment of ALS and set the foundation for future studies designed to identify drugs that increase the levels of this protein as the basis of a new treatment for ALS.
 Enhancing mitochondrial transport as a potential therapeutic strategy for ALS
Enhancing mitochondrial transport as a potential therapeutic strategy for ALS
Thomas Schwarz, Professor of Neurology and Neurobiology, Harvard Medical School and Boston Children’s Hospital
Neurons have an intense requirement for energy to power their electrical signals and support their survival. This energy is supplied by mitochondria. The motor neurons that degenerate in ALS are large, with axons extending for up to a meter from the spinal cord to muscles in the extremities. Energy, and therefore mitochondria, are required along this entire length. Because the genes that encode most mitochondrial proteins are in the motor neuron’s nucleus in the spinal cord, keeping a healthy supply of mitochondria in the axon requires the movement of mitochondria up and down the axon. Recent studies have shown that the transport of mitochondria is compromised in several neurodegenerative diseases, including ALS. Thus, insufficient transport of mitochondria may contribute to the degeneration of ALS motor neurons. Conversely, we have hypothesized that enhancing the movement of mitochondria in axons may help those neurons survive. To this end, we have screened for small molecules that can enhance mitochondrial transport in cultured rodent hippocampal neurons and have identified the cellular targets of those molecules. We will now ask whether these same compounds and the cellular pathways they alter are capable of acting in human motor neurons. We will use neurons derived from ALS-patient stem cells to characterize their transport defects and determine whether compounds from our screen can restore normal levels of mitochondrial movement in these neurons.
2016-2017 Awards
 Neuronal size as a stressor in ALS: a new hypothesis about motor neuron degeneration
Neuronal size as a stressor in ALS: a new hypothesis about motor neuron degeneration
Marc Kirschner, Professor of Systems Biology, Harvard Medical School
Jeff Lichtman, Professor of Molecular and Cellular Biology, Harvard University
Due to vertebrate body size and shape, neurons projecting from the spinal cord and brainstem to muscle fibers greatly vary in size. The metabolic costs for individual neurons to maintain large cytoplasmic loads or large electrical burdens are essentially unexplored. However, ALS clearly affects large neurons and spares small neurons, suggesting that cell size is a stressor for neurons. In motor neuron disease, neuron loss has a striking effect on cell size: the remaining neurons sprout terminal branches to reoccupy vacant sites within muscles previously occupied by projections from the lost neurons. Collaborative work by the labs of Drs. Lichtman and Kirschner reveals that this sprouting causes the remaining neurons to add significant cytoplasm, which may further stress the neurons and cause a cell death cascade. In this project, the labs will work together to study neuron size and metabolic load in mouse models of ALS, and determine if ALS-prone motor neurons can be rescued by strategies that restrict sprouting. Their study will be the first attempt to learn how neuron size affects ALS and may provide entirely new avenues for therapy.
 Strengthening the foundation for ‘in the dish’ studies of patient-derived ALS motor neurons
Strengthening the foundation for ‘in the dish’ studies of patient-derived ALS motor neurons
Allon Klein, Assistant Professor of Systems Biology, Harvard Medical School
An important part of studying any disease is accurately modeling it in the laboratory. The study of human nervous system disorders has been aided significantly in the past decade by the development of induced pluripotent stem cells (iPSCs)—which allow researchers to take readily-accessible cells (such as skin cells) from patients, reprogram them into stem cells, and then apply ‘differentiation’ protocols that make those stem cells into the cell type of interest—such as motor neurons for ALS studies. But currently there is a great deal of variation in the range of protocols used, the variety of cell types produced by each protocol and the stages of neuronal development modeled. Dr. Klein’s lab will develop a general framework for defining the cell states emerging from iPSC-motor neuron differentiation protocols, employing “inDrops”—a powerful droplet microfluidic barcoding technology developed in their lab, which enables rapid genome expression profiling of tens of thousands of cells in a single experiment. The information gleaned from such studies will ultimately help the team determine which protocols reliably produce specific cell types most relevant for ALS disease progression and strengthen, for the entire field, the foundation for comparative studies of healthy vs. ALS patient-derived cell cultures.
 Molecular studies of a receptor protein which may spark the design of new ALS therapeutics
Molecular studies of a receptor protein which may spark the design of new ALS therapeutics
Andrew Kruse, Assistant Professor of Biological Chemistry and Molecular Pharmacology, Harvard Medical School
The sigma-1 receptor is an enigmatic membrane receptor found in all vertebrates, including humans. Unlikemost other receptors, it does not belong to any major protein family but instead is unique in the human genome. Sigma-1 has long been known to have protective effects in models of cell stress, and recently a connection to ALS has emerged from studies of human genetics and mice. In particular, defects in the sigma-1 receptor gene can cause ALS-like neurodegenerative disease in humans, and in mouse models of ALS, deletion of the sigma-1 gene exacerbates the disease. Other research has shown that sigma-1 activators can prolong lifespan and delay the onset of disease symptoms. Despite these encouraging results, current sigma-1 activators often have off-target effects on other receptors, making them poor candidates for therapeutic use in humans. Rational drug development for the sigma-1 receptor has been hampered by the near complete lack of molecular-scale information regarding its function. Dr. Kruse’s lab recently addressed this gap by determining the first high-resolution molecular structure of this receptor. In this project, they will elucidate the molecular basis for sigma-1 activation and develop novel activators of this receptor to use both as research tools and therapeutic candidates. The ultimate goal is to shed light on sigma-1’s role in ALS development and evaluate its prospects as a drug target.
 Molecular studies of transporter proteins which may be reducing the efficacy of ALS drugs
Molecular studies of transporter proteins which may be reducing the efficacy of ALS drugs
Maofu Liao, Assistant Professor of Cell Biology, Harvard Medical School
There are often discrepancies in different stages of ALS drug development. It is hard to translate ALS drugs developed in the dish into therapies that work in animal models, and harder still to turn preclinical successes into drugs that work in patients. Mounting evidence suggests that these discrepancies may result from the previously overlooked issues of drug bioavailability (how much of the drug actually gets to the nervous system site of action) and disease-driven pharmacoresistance (a diminished response to the drug that occurs due to disease-driven changes in the patient’s body). The ATP-binding cassette (ABC) transporter proteins play critical roles in both these phenomena. The ABC proteins found at the blood-brain and blood-spinal cord barriers effectively protect the central nervous system by extruding a broad range of foreign or neurotoxic substances—but they also limit drug penetration. Furthermore, ABC efflux transporters are present at increased levels in various central nervous system disorders, including ALS—leading to the pharmacoresistance problem. To learn precisely how ABC transporters contribute to pharmacoresistance in ALS, Dr. Liao’s lab will use an advanced structural biology method called single particle cryo-electron microscopy to study the structure and function of these transporters. Their work will shed light on drug-transporter interactions and help in the development of novel ALS therapeutics that block or evade the ABC efflux transporters.
 Understanding how a common ALS mutation disrupts splicing—an essential step in the production of proteins from DNA
Understanding how a common ALS mutation disrupts splicing—an essential step in the production of proteins from DNA
Robin Reed, Professor of Cell Biology, Harvard Medical School
Recently, mutation of a gene designated C9ORF72 was identified as the most common cause of ALS. The mutated form of this gene gives rise to proteins that are toxic to cells, and these toxic proteins cause disruption of an essential step in gene expression known as splicing. Notably, splicing disruption is also observed with other ALS-causing genetic mutations. Dr. Reed’s lab is interested in better understanding the link between ALS and splicing problems. In this project, her team will determine how splicing is disrupted in ALS caused by the C9ORF72 mutation. They have preliminary data revealing that the toxic proteins produced by mutant C9ORF72 associate with an essential component of the cellular machinery required for splicing. They now plan to determine whether the toxic proteins interfere with the normal functioning of this splicing component in a test tube-based assay, and as well as in neuronal cells generated from ALS patient stem cell lines which harbor the C9ORF72 mutation. Among the many critical questions to be answered is the question of whether the splicing component of interest directly interacts with the toxic proteins present in the ALS patient cells. The ultimate goal is to learn whether splicing components may be therapeutic targets in ALS.
 Matching gene activity to pathology at the single cell level in patient-derived ALS motor neurons
Matching gene activity to pathology at the single cell level in patient-derived ALS motor neurons
Clifford Woolf, Professor in Neurology and Neurobiology, Boston Children’s Hospital and Harvard Medical School
One of the major mysteries of ALS is why motor neurons in particular are susceptible to cell death. One way to tackle this problem has been to develop disease-in-a-dish models using patient-derived stem cells (iPSCs) as a means to make motor or other neurons and then identify some alteration in the structure or function of the patient motor neuron. Using this approach in a collaboration with Drs. Brian Wainger (now at MGH), Kevin Eggan(Harvard University) and Bruce Bean (Harvard Medical School, also an HBI Seed Grant Awardee), Dr. Woolf found that ALS motor neurons derived from patients with the familial form of the disease are hyperexcitable. This means, essentially, that their electrical activity is more susceptible to a certain type of fluctuation (an increase in membrane voltage) that might make them more vulnerable to cell death. The likely cause of this hyperexcitability was narrowed down to a reduction in potassium ion flow across the cell membrane.
The question Dr. Woolf’s lab will now pursue with this seed grant is which individual ion channel subtype is selectively expressed at different levels only in ALS motor neurons to lead to hyperexcitability. To do this, the lab will couple recordings of excitability in individual ALS and control motor neurons with the level of gene expression in these same neurons using Next Generation single cell sequencing technology. This will provide a very fine grained insight, one cell at a time, into the relationship between function and gene expression. Preliminary data indicate that reduction in a potassium ion channel might be a factor. Once a factor(s) of interest has been determined, Dr. Woolf’s team will knock the corresponding gene out in healthy motor neurons to see if those neurons develop any ALS-like dysfunction. Conversely, they will test if normalizing expression of the gene back to control levels can rescue ALS motor neurons from their death trajectory.
 Cell biological studies of RIPK1—an ALS drug target nearing entry into clinical trials
Cell biological studies of RIPK1—an ALS drug target nearing entry into clinical trials
Junying Yuan, Professor of Cell Biology, Harvard Medical School
The enzyme RIPK1 is a key mediator of inflammatory signaling, as well as multiple forms of cell death. Thus, inhibiting RIPK1 might block cell death and neuroinflammation simultaneously. Inhibition of RIPK1 has shown efficacy in protecting against multiple animal models of neurodegenerative diseases, including ALS. Dr. Yuan’s lab will investigate the involvement of RIPK1 in the pathology associated with various human ALS mutations, as well as biomarkers for RIPK1 activation, using mouse models of the human ALS mutations. This work may provide important cell biological foundations to prioritize the testing of a RIPK1 inhibitor in clinical trials, including key insights into patient stratification—in other words, revealing the biological profile of patients who might benefit most from this type of drug.
2015-2017 Awards
 Pharmacological Dampening of Motor Neuron Hyperexcitability in a Mouse Model of ALS
Pharmacological Dampening of Motor Neuron Hyperexcitability in a Mouse Model of ALS
Bruce Bean, Robert Winthrop Professor of Neurobiology
The death of motor neurons in ALS is preceded by neuronal hyperexcitability, which may promote cell death by allowing excess calcium entry. Using a mouse model of ALS, we will attempt to identify new pharmacological agents that can reduce hyperexcitability without disrupting normal neural function. Recording the electrical activity of motor neurons in spinal cord slices from mice, we will explore how specific ion channels control motor neuron firing in normal and pathological conditions and use this information to choose ion channels to target by pharmacological agents. Initial drug candidates include already known potassium channel-enhancing agents, which reduce neuronal hyperexcitability. These drugs, including retigabine, chloroxazone, and EBIO, are used to treat epilepsy and other diseases. Other candidates will emerge from a better understanding of how firing is regulated by specific channel types in both wild-type and mutant neurons.
The lab has extensive experience in ion channel pharmacology in the context of epilepsy and pain, two other disease states that involve hyperexcitability of neurons, but we are new to ALS research. We are excited that this opportunity challenges us to use our base of knowledge to help devise new pharmacological approaches to ALS. The seed grant will allow Dr. Wenqin Hu, a postdoctoral fellow with extensive experience in studying excitability of cortical neurons, to shift her focus to spinal motor neurons. She became very enthusiastic about this project while performing trial experiments to get preliminary data for the proposal, and the seed grant is likely to be instrumental for her possible career shift to ALS research.

 Misfolded Protein Degradation via the Ubiquitin-Proteasome Pathway in ALS
Misfolded Protein Degradation via the Ubiquitin-Proteasome Pathway in ALS
Daniel Finley and Steven Gygi, Professors of Cell Biology
It is thought that the motor neurons affected in ALS are poorly equipped to neutralize toxic, misfolded proteins. Mutations in the gene encoding the SOD1 protein, the first well-defined ALS mutations, provide a good example. SOD1 mutations convert this protein, which is beneficial in its normal state, into an altered shape that is toxic to the cell. However, all cells contain complex machinery to detect and destroy misfolded proteins. This can be thought of as a quality control system similar to those in factories that monitor the integrity of their products.
Our view that protein quality control pathways are critical in ALS has been strengthened greatly in recent years by the finding that ALS can be caused by defective components of the quality control pathway itself. Furthermore, we have shown that enhancing the activity of the quality control pathway using non-toxic small molecules can eliminate some misfolded ALS proteins. Our experiments aim to determine which misfolded ALS-related proteins are eliminated via a specific quality-control pathway already implicated in ALS: the ubiquitin-proteasome pathway that employs the UBQLN2 receptor. We will do this using new technologies that allow comparison of the full set of proteins produced in normal and pathological cells. The ultimate goal of this work is to find ways to strengthen this pathway, so it can neutralize toxic proteins more effectively in the motor neuron.
 Control of Endosomal Trafficking in ALS
Control of Endosomal Trafficking in ALS
Wade Harper, Professor of Cell Biology and Bert and Natalie Vallee Professor of Molecular Pathology
ALS is a progressive disease in which lateral motor neurons die, leading to an inability to control muscle function. Recent genetic analysis of ALS patients has revealed several candidate genes with potential roles in the choreographed movement of molecules and organelles within the cell, known as “trafficking.” Trafficking is particularly challenging for spinal motor neurons because specific proteins and other cellular cargo must be delivered down an axon to precise locations up to a meter away from the cell body where they are made. New therapies for ALS could hinge on identifying important cargo and the key machinery that is defective in the delivery process. A central element of cellular trafficking is the endosomal system, a complex compartment inside of a neuron that transports proteins around the cell.
Defects in the endosomal system have been implicated in ALS, but its normal function in motor neurons and the way it breaks down in ALS remain poorly understood. We are studying a network of interacting proteins whose genes are mutated in ALS. A central protein in this network is called NEK1. Our evidence suggests that NEK1 may regulate two components of the endosomal system: one promotes endosome maturation and the other controls which specific proteins are captured by the endosome and where they are routed. Our experiments aim to determine how NEK1 works normally and how patient-derived mutations in NEK1 contribute to motor neuron pathology in ALS.
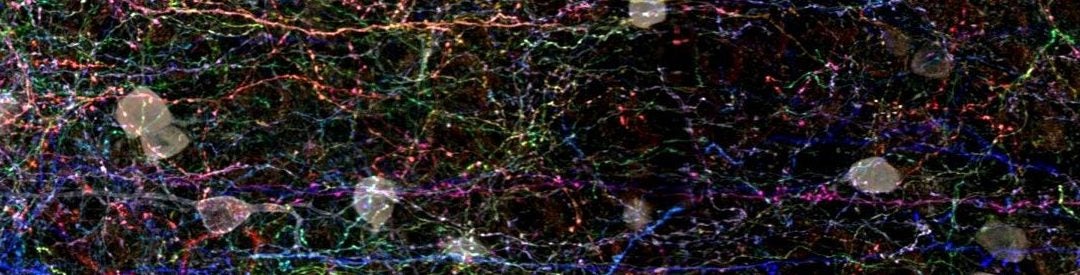
Banner image shows Brainbow staining of a section of brain tissue, courtesy of the labs of Takao Hensch and Jeff Lichtman